By Lambert Strether of Corrente.
I had a recent conversation with a friend who gave an exhaustive, blow-by-blow description of her recent encounter with the best health care system in the world — it was bad, very bad — and she pointed out to me that while I’ve written in some detail on ObamaCare and health insurance companies, I haven’t really ever taken a look at doctors and hospitals, and they’re also part of the problem. But those are big topics; health care was, after all, 17.1% of GDP in 2014 (13.1% in 1995).
So I thought I would try to limit my scope, and take a look at medical coding, partly because I know something of taxonomies, but also because the medical coding dataflow unites patients, providers (doctors, hospitals), and payers (health insurance companies, and government), so medical coding is a vantage point from which to view the entire horrid, lethal system.
First, I’ll refresh readers’ memories on phishing equilibria, then provide with a potted history of medical coding, including a classification of medical coding errors (?) in the United States today, examine consumer-driven (non-)solutions to fix coding errors, and conclude.
Phishing Equilibria
From my review of Akerlof and Shiller’s Phishing for Phools, November 25, 2015:
As businesspeople choose what line of business to undertake — as well as where they expand, or contract, their existing business — they (like customers approaching checkout) pick off the best opportunities. This too creates an equilibrium. Any opportunities for unusual profits are quickly taken off the table, leading to a situation where such opportunities are hard to find. This principle, with the concept of equilibrium it entails, lies at the heart of economics.
The principle also applies to phishing for phools. That means that if we have some weakness or other — some way in which we can be phished for fools for more than the usual profit — in the phishing equilibrium someone will take advantage of it. Among all those business persons figuratively arriving at the checkout counter, looking around, and deciding where to spend their investment dollars, some will look to see if there are unusual profits from phishing us for phools. And if they see such an opportunity for profit, that will (again figuratively) be the “checkout lane” they choose.
And economies will have a “phishing equilibrium,” in which every chance for profit more than the ordinary will be taken up.
We might summarize Akerlof and Shiller as “If a system enables fraud, fraud will happen,” or, in stronger form, “If a system enables fraud, fraud will already have happened.”[1] And as we shall see, plenty of “opportunities for unusual profits” exist in medical coding.
Medical Coding from the Black Death to the Present Day
Medical coding is said to have begun in England as a way of tracking (and avoiding) epidemics, especially the Black Death. Here is a weekly “Bill of Mortality” from that time:
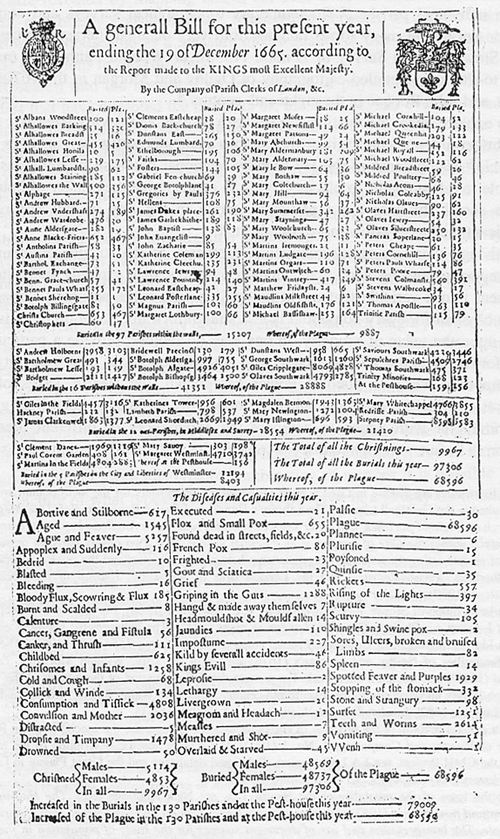
The London Bills of Mortality were published weekly, and as of 1629 included the cause of death. Information was collected by parish clerks in various geographical areas. In order to determine which areas had the most cases of plague, Londoners purchased copies of the Bills and tracked the spread of the disease from one parish to another in order to avoid it.
Causes of death found in the Bills include diseases recognized today, such as jaundice, smallpox, rickets, spotted fever and plague. Other conditions have creative descriptions like “griping in the guts,” “rising of the lights” (croup), “teeth,” “king’s evil” (tubercular infection), “bit with a mad dog,” and “fall from the belfry.”
“Griping in the guts.” I get that one a lot. Fast forward to the 21st century, where we use a far more complicated classification system, the International Statistical Classification of Diseases and Related Health Problems (ICD-10), focused on morbidity instead of mortality. The ICD is maintained by WHO:
ICD is used by physicians, nurses, other providers, researchers, health information managers and coders, health information technology workers, policy-makers, insurers and patient organizations to classify diseases and other health problems recorded on many types of health and vital records, including death certificates and health records. In addition to enabling the storage and retrieval of diagnostic information for clinical, epidemiological and quality purposes, these records also provide the basis for the compilation of national mortality and morbidity statistics by WHO Member States.
Right here in WHO’s genteel prose we can see the potential for phishing. Why? Because some of the players (nurses, researchers, patient organizations) are not motivated by profit, while others (insurance companies) are, and still others (doctors, coders, information technology workers, policy makers) may be, or may not be. Medical coding is, in other words, conflicted at its core, because it serves players driven by profit, and players not driven by profit. How will the balance be struck? Surgeon Martin Makary answers:
“Incidence rates for deaths directly attributable to medical care gone awry haven’t been recognized in any standardized method for collecting national statistics,” says Martin Makary, professor of surgery at Johns Hopkins University School of Medicine. “The medical coding system was designed to maximize billing for physician services, not to collect national health statistics, as it is currently being used,” Makary says.
Beyond its conflicted role, medical coding in the United States is enormous and complex:
The International version of ICD should not be confused with national modifications of ICD that frequently include much more detail, and sometimes have separate sections for procedures. The US ICD-10 Clinical Modification (ICD-10-CM), for instance, has some 68,000 codes.[6] The US also has the ICD-10 Procedure Coding System (ICD-10-PCS),[7] a coding system that contains 76,000 procedure codes that is not used by other countries.
(By comparison, the North American Industry Classification System (NAICS), used to classify all forms of business, contains only 2196 codes (from 11, “Agriculture, Forestry, Fishing and Hunting,” through 928120, “International Affairs.”)
A reporter from the Weekly Standard, of all places, gives a sense of the training (see Appendix) required to even understand the codes:
On a foggy Thursday morning in early January, 30 medical coders gathered in a nondescript meeting room on the third floor of the downtown Hyatt Regency in Jacksonville. They paid between $585 and $985 each to attend a two-day “boot camp” on the new codes taught by Annie Boynton, from the American Academy of Professional Coders. On the black cloth covering each table were the day’s necessities: a Hyatt Regency pad of paper and pen, a coffee cup and saucer, a jar full of hard candy, a glass and a sweating metal pitcher filled with ice water. At each place, students found a thin spiral book—the “ICD-10-CD General Code Set Manual” for 2014—and a six-pound, phone-book-thick “ICD-10 Complete Draft Code Set.”
The reporter also gives a reason why our coding is exceptionally complex:
Other developed countries began their implementation of ICD-10 some 20 years ago, after the World Health Organ-ization released its basic version of the new code set. But their versions of ICD-10 won’t be nearly as complicated as the U.S. version. Boynton says that only 10 other countries use the codes for reimbursements—one of the main functions of ICD-10 in the United States. And payment systems elsewhere are far less complicated, in part because there is usually just one payer: the government.
The multiplicity of payers in the U.S. system partly explains why ICD-10 will be vastly more complicated here. But, paradoxically, if government explains the simplicity of ICD-10 codes elsewhere, government largely explains the complexity of the ICD-10 codes here. And those codes are complex.
So, yet again, the United States pays an exceptionally high price for its fealty to neoliberal, markets uber alles, ideology.
Medical Coding and Phishing Equilibria
Here is the medical coding process, from the coders perspective, as described by MB-Guide, a site for aspiring medical coders:
Successful medical coders learn and follow coding guidelines and use them to their benefit. Often if a claim is denied incorrectly, medical coders and billers use coding guidelines as a way to appeal the denial and get the claim paid.
Hmm. “Their” benefit. Here are the guidelines:
The specificity of the diagnosis code: Each diagnosis code has to be coded to the highest level of specificity, so the insurance company knows exactly what the patient’s diagnosis was.
The correct reporting of procedure codes: There are too many rules and regulations to go into here. There are specific ways to code each visit, which help identify the service that was provided to the patient.
Reasonable and customary charges: Regulating bodies also suggest that providers charge only “reasonable and customary” rates for their services. This prevents over-inflation of medical fees.
Procedure code modifiers: When certain procedure codes are sent on the same claim form, they sometimes require medical billing modifiers, which help differentiate between the codes that were charged on the date of service.
I’ve helpfully underlined places where an “unusual opportunity for profit” might be spotted and amplified; after all, it’s not the coder’s job to set policy in borderline cases; that’s for management.
I can think of three coding decisions where phishing equilibria might settle in: Impedance mismatch, miscoding, and upcoding.
An “impedance mismatch” would happen when one coding system has to be mapped to another. Before there was ICD-10, there was ICD-9, and millions of records (presumably) were recoded, in a process of data conversion. The problem:
Given the significant expansion and details in ICD-10 codes, it is not always possible to find a unique ICD-10 code to match exactly an ICD-9 code. In about 20% of cases, there are multiple ICD-10 codes for one ICD-9 code, or multiple ICD-9 codes for one ICD-10 code, or there is simply no exact match between the two systems.
So how was the judgement call made? Clearly, an opportunity for a phishing equilibrium.
“Miscoding” is the equivalent of a typo or a copy editing error. The Denver Post gives a horrific example:
Miscoding Fictions, frauds found to abound in medical bills
A pair of transposed digits in a medical identification number was the difference between insurance coverage for Mike Dziedzic and the seemingly never-ending hounding for payment by the hospitals that cared for his dying wife.
The astute eye of a medical billing advocate who Dziedzic hired for help caught the innocuous mistake — the sole reason his insurance company had refused to pay more than $100,000 in claims that had piled up and why collectors were now at his doorstep.
Had it remained unnoticed — as often happens to patients faced with daunting medical debt — Dziedzic said, he most surely would have lost his Rifle home, his way of life and had little choice but to live in bankruptcy.
Finally, there’s “upcoding,” and if you are reminded of “upselling” you are exactly right. The Center for Public Integrity:
But the Center’s analysis of Medicare claims from 2001 through 2010 shows that over time, thousands of providers turned to more expensive Medicare billing codes, while spurning use of cheaper ones. They did so despite little evidence that Medicare patients as a whole are older or sicker than in past years, or that the amount of time doctors spent treating them on average was rising.
More than 7,500 physicians billed the two top paying codes for three out of four office visits in 2008, a sharp rise from the numbers of doctors who did so at the start of the decade. Officials said such changes in billing can signal overcharges occurring on a broad scale. Medical groups deny that.
The most lucrative codes are billed two to three times more often in some cities than in others, costly variations government officials said they could not explain or justify. In some instances, higher billing rates appear to be associated with the burgeoning use of electronic medical records and billing software.
Now, I’ll be the first to admit that I can’t quantify the impedance mismatches, the miscoding, and the upcoding. Regardless, medical coding is the key dataflow in the healthcare system:
“Roughly $250 billion is moving through those codes,” [says Steve Parente, professor of finance at the Carlson School of Management at the University of Minnesota]. On top of that, about 80% of medical bills contain errors, according to Christie Hudson, vice president of Medical Billing Advocates of America, making already-expensive bills higher. Today’s complex medical-billing system, guided by hundreds of pages of procedure codes, allows fraud, abuse and human error to go undetected, Hudson says. “Until the fraud is detected in these bills … the cost of health care is just going to increase. It’s not accidental. We’ve been fighting these overcharges…they continue to happen and we continue to get them removed from bills.” These errors, which are hard to detect because medical bills are written in a mysterious code, can result in overcharges that run from a few dollars to tens of thousands.
That “mysterious code” is (now) ICD-10, and it’s the mystery plus the profit motive that creates the phishing equilibrium. Kaiser Health News quotes the Denver Post:
Experts say there are tens of thousands more like Dziedzic across the country with strangling medical debts. Medical Billing Advocates of America, a trade group in Salem, Va., says that eight of 10 bills its members have audited from hospitals and health care providers contain errors. It’s estimated that at least 3 percent of all health care spending – roughly $68 billion – is lost to fraud and billing errors annually. Some say new reform laws will only make things worse.” Others say that errors occur largely because of “the complexity of deciphering bills and claims weighted down by complex codes.”
Even if the “trade group” is talking it’s book, it’s still quite a book. NBC:
Accounts of medical billing errors vary widely. While the American Medical Association estimated that 7.1 percent of paid claims in 2013 contained an error, a 2014 NerdWallet study found mistakes in 49 percent of Medicare claims. Groups that review bills on patients’ behalf, including Medical Billing Advocates of America and CoPatient, put the error rate closer to 75 or 80 percent.
Gee, I wonder if the errors are randomly distributed?
Neoliberal “Consumer”-Driven Solutions
My guts have started to gripe, so I won’t go into detail about how you too, the citizen consumer, can learn medical billing codes if you want to dispute your bill. See this cheery post from NerdWallet on “How to Read Your Medical Bill:
Once you have the itemized medical bill for your care, you’re ready to analyze it for mistakes and overcharges.
Your medical bill is going to be chock-full of codes and words you may not understand, so the first step is gathering resources that will translate them into plain English.
Nerdwallet also includes this helpful image of a medical bill[2]:
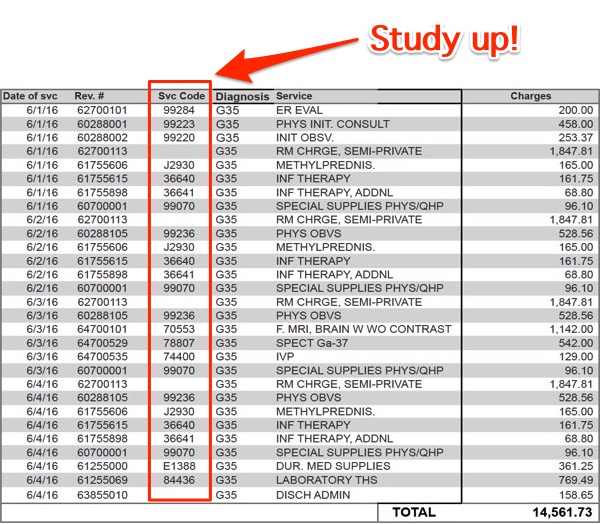
At this point, we recall that professionals paid between $585 and $985 to “gather resources,” one of which was telephone book-sized documentation. That’s quite a “tax on time.” (This FOX article also includes a good checklist of ways to dispute your bill: “The No.1 rule that we tell individuals is never pay the summary bill.”)
Conclusion
Wouldn’t it be nice if we had single payer? A much unappreciated universal benefit of Medicare for All is that none of us would have to learn medical coding to successfully dispute a bill![3] And an entity with some clout — the state — would be doing the disputing for us, on our behalf. Readers, have any of you had experience with this process? Either as a citizen consumer, or — even better! — as a coder, yourself?
NOTE
[1] There are more forms of phishing than fraud, but this crude summary will do for our purposes now.
[2] Reader TheBellTolls points out the column of codes is HCPCs/CPTs (procedure coding), not ICD10. The point remains, indeed is implified (especially impedance mismatch).
[3] Yes, I know Medicare suffers from a neoliberal infestation. But we have to start somewhere…
When I was researching this article, I searched on “medical coding.” Most of the first page of Google’s search results was taken up ads for medical coding training. From MB-Guide.org:
Considering a career change? Have you thought about the medical billing and coding field?
These industries helps millions of medical professionals and patients each year, and offer secure employment.
Medical billers and coders handle the complicated world of insurance claims for healthcare professionals. Without a constant stream of insurance claim revenue, healthcare facilities would quickly stop working. Billers and coders play a vital role in keeping things ticking.
Salary data from AAPC reveals that the more AAPC credentials an individual carries, the higher their annual salary. The average annual salary in 2015 of members with:
1 credential (any credential) was $46,899
2+ credentials (any credentials) was $58,399
3+ credentials (any credentials) was $65,643
And it’s interesting what there are credentials for, and what there are not credentials for:
The little-known field of medical-billing [patient] advocacy remains in its infancy, largely because there are no specific certifications or schooling necessary. MBAA offers in-home study courses and Sarah Lawrence College in Bronxville, N.Y., offers a masters program in health advocacy — there are even courses to learn the special coding necessary for medical billing — but just about anyone can hang a shingle and say he or she is an advocate.
Probably because it’s better to become a single payer advocate than a medical billing advocate.


One useful adjunct to the coding discussion concerns other billing details such as meds. There is wide variability in prices charged, and when you see $160 for a single pill (e.g., Hexabrix) or $26 for a single Tylenol, then something is not right. Of course, that does not include any allocation for nurses, pharmacy or other potential costs, since those are rolled into other line items to decipher. When hospital billing reps are asked about the reasonability and basis of their charges, they spout the canned line about being in line with their local competitors.
Why not have some program with mutual insurance companies, removing in theory some of the profit that is driving the typical health care insurers?
The same line that is used in medical malpractice: “Standard of Care”……covers lots or territory or “sins”.
Most services don’t get paid based on ICD, they get paid based on HCPCs/CPTs (healthcare procedure codes) which is what is shown in the nerdwallet image. Also revenue codes will be used for facility services (such as the room charge in image).
ICD-Diaganosis codes just tell you what conditions the provider diagnosed you with. ICD-Procedure codes are sometimes used for payments but usually only on inpatient claims.
_________________________________
Additionaly, coding also affects “risk adjustment” in Medicare Advantage and ACA payments and this form of payment does use ICD codes. They use the codes on the claims to determine how “sick”(has conditions that will cost more) each member is and give insurers more or less money based on the average risk scores of their members. Since it relies on coding this system is also subject to gaming.
In Medicare Advantage this is done relative to non-Medicare Advantage population, so if the MA plans are upcoding they get more money from Federal government. In 2010 CMS was given the ability to use some adjustment factors to MA payments to address the issue but I don’t really know how effective it is.
In ACA this is done relative to all the other insurers in the individual/small group market(so all the money is changing hands between the insurers). More established plans generally do better since they have more data on members from before ACA to make sure they get coded in addition to resources they probably built from Medicare Advantage. This ends up disadvantaging smaller and newer plans like co-ops.
_____________
Thanks. I meant to distinguish the procedures codes and accidentslly cut that para!
This is very interesting, Lambert, as my experience with medical coding began in a very large medical records department in Los Angeles in the mid-80’s. California (under Governor Reagan) was the originator, I believe, in linking diagnostic codes to billing charges. The training of coders can (and often is) very indifferent – they usually have no medical background whatsoever, and make a lot of executive decisions throughout the day. For instance, we had a significant problem with ‘false starts’ ER admissions of pregnant women. The coders unilaterally decided that since no baby was delivered, no charges could be billed. And so on.
Coming from the other direction as a (now) chronic patient – I recently visited a new neurologist, who had enormous confidence in his ability to making lightning diagnoses (with negligible examination). When it came time to write up some scrips, he turned to a small hand-held device, which contained the new ICD-10 diagnostic codes. ‘Traumatic Brain Injury’ he intoned. The device didn’t recognize the diagnosis. He scrolled through – it was not there. He began degrading the diagnosis – how about ‘brain injury’? No dice. How about ‘concussion’ (actually not the case) – Bingo. Thus I am now in the system under an incorrect diagnosis because ICD-10 – as encoded in the device cannot accommodate a brain injury DX.
You are like a dog with a bone on this Lambert.
I appreciate the efforts taken to keep us informed on the sickness industry in the USA. Every single person who needs meds, health intervention/advice is having his/her pockets fleeced and given a shit product in return.
Very little of what I read here on NC encourages me to travel to the US again. Which is a real shame.
> You are like a dog with a bone on this Lambert.
Thank you!
A little over 30 years ago a close relative underwent brain surgery. Recovery lasted about a half-hour. Then, after 22 days in Neurosurgical Intensive Care, death with sepsis as the proximate cause, brain stem damage as the ultimate cause. The “bill” was at least 500 pages long. The insurance provider (from a good union contract) told the hospital, surgeon, and hematologist-oncologist there would be a line-by-line audit of the entire file. Hospital and the physicians responded, “How about a 50% discount?”. Insurance provider said, “Okay.” Life insurance still had to provide a very large chunk of the deceased’s share. And that was that. I shudder to see the equivalent “paperwork” today. The best health care system in the world. Then and now. The previous occupant at 1600 Pennsylvania will have a lot to answer for. Well, no, he won’t, but one can hope.
That’s a terrible story.
I think the itemised bills, with every towel, tissue and glove ‘accounted for’, are a feature of the system.
Never had a bill from a hospital, but had some from lawyers. The itemised bill is a way of showing evidence – that the bill is right as we did use 78 disposable gloves etc.
What gets lost in the detail is the large disconnect between cost and price. And, when you can’t negotiate on price, because you have no leverage, you are a price taker.
What singe payer brings to the table is a single consumer, a government that can set sensible ceilings on prices.
The US will never get it though, the medical-pharma-insurance group is too powerful and has a lot of money to influence political choices.
And the lie that taxes fund government spending will continue to be put up as the reason why we can’t have nice things.
In 2010 I was disputing the itemized charges on my wife’s maternity bills (which included $12 advil pills). I went the administrative office, and they lady at the front kept tying to justify number that didn’t add up properly in the bill summary.
I started getting irritable, and so the lady at the front went to the lady (manager) in the back who came back up front with a new summary bill number that still didn’t add up with the itemizations, but was about 30% cheaper so at that point I relented and agreed to pay that value.
Not too different than a trip to the car dealership if you ask me.
Make no mistake, the healthcare industry is a business first and foremost, the goodness of doctors noble intentions when they got into the profession not withstanding.
Icd-10 is just another piece of bullshit uncompensated work that is completely separate from the actual work of being a physician, i.e., taking care of patients.
This is what happens when a third party, the payor, interposes itself between the patient and the physician and then starts using the power of the purse to call the shots.
The medical record has gone from a method of communicating with the other members of the care team and memorializing your thoughts for future patient care to a billing, cya and surveillance device. So it is full of bullshit and has become an impediment to patient care. It’s a literal dumping ground that never gets cleaned.
I don’t know the solution. You can say single payor, but if you’ve ever worked in the VA then you know that’s a recipe for disaster. There are no incentives for working hard and the bureaucratic culture is pervasive and unbearable. I suppose it won’t matter when we are all replaced by robots and algorithms.
I started to think this even when I was studying to be a nurse at uni. And the advice I got from other nurses was the same. CYA! I work in Australia, where we have a Medicare system which is mostly the single payer.
What’s interesting is the beds available for different diagnoses. On some mental health units, for example, the most lucrative is for people with eating disorders(in terms of how much the hospital gets). Sometimes 25% of the beds in some adolescent and adult units. But, I wasn’t aware of the kind of phishing happening that Lambert is indicating. Does it skew people’s admission policies though? Hard to tell.
The big money probably lies with oncology-I remember giving meds on a haemotology ward that were about $5000 a pop.
There was a Link in NC some years ago about a teenage girl (New York?) who wanted to refuse treatment for a lymphoma DX. (She likely knew her parents could not afford the medical treatment.) Some NC commenters suggested she was being foolish. I replied that having BTDT, the cost of ONE round of chemotherapy (the drug alone) is ~$17,000 (No shit, Sherlock!). And the (un-fun) initial procedure usually involves 5-6 treatments two weeks apart, along with corollary treatments involving PET/CT scans, that will be ongoing for five years.
Obviously, I made the choice to endure the treatment, but the final tab was well over $100,000. (Worth the price of admission to the future, if you have excellent medical insurance.)
We’re at the point where the algorithms are being offered as a service for a fee to assist the physician’s practice (the meat farm out front of the cage with the sliding glass) in adding billable codes to an office visit. Analyse the patient’s history, then compile a list of things to ‘discuss’ or tests to run at next visit. Then sell it as preventive, for the patient’s benefit. We’re looking after you in your best interest.
Time for MD school to offer a semester class on killing the billing taxonomy.
> We’re looking after you in your best interest.
I don’t doubt it, but do you have a link?
I never posted on it, because ObamaCare has so much else to post on it, but ObamaCare incentivized “wellness” programs, even though the field had no demonstrated medical benefit. Sounds very much like a useful way for medical practices to upsell, as you say. And it fits nicely with the EHR stuff that Obama actually funded with stimulus money, if you can believe it.
Medical bills are a nightmare. I am a retired military reservist so I have free insurance, but the hospital evidently fights the insurance company over every nickel and dime. I went in for a simple procedure but the bills just kept on coming. I actually filed a formal grievance with Tricare over the multiple screw-ups committed by my so-called “surgeon”—-a lot of good that did me. The hospital just kept sending me bills for like $25 or $30 once a month for two years. The bill never stated what I was being billed for. Maybe the “surgeon” was mad at me for filing the grievance, so she resolved to get every dollar she could from me.
Finally I called up the hospital and told them I wasn’t going to pay any more of these bills and their response was simply: “OK.” I guess their policy was to keep sending bills forever until the customer finally puts his or her foot down. Like a lot of the local populace, I resolved to never set foot in that hospital again—-for any reason.
The whole US medical system is insane. That’s why I support medicare for all, even though I would in effect be losing the relative advantage of my free medical insurance.
This was a nightmare for me, and I was fairly young and healthy. The nightmarishness is multiplied manifold, of course, when the patient is old, drugged up, nearly or completely senile, in pain, and/or dying, which is often the case.
ex-in law was intended to be held hostage and converted to a nursing home this religious based large hospital in brooklyn had just opened up before 9-11…not that in law did not do her part to make life interesting by acting the crazy child and pulling out her medical attachment to make them redo them over and over…she tended to insist she was “always” ill and taken to the emergency room via ambulancee…
did her best fred sanford on a regular basis(this is the big one…)…
except this time she actually caught something in the emergency room….after a few weeks of her discooperationalisms, they were pushing to peg her…and after the hospital was done slowly working it, my ex reluctantly agreed as my ex worked for a major nyc based hmo dealing with hospital billing disputes and had arranged for a transfer to a specialized respiratory care unit inside a hospital on Roosevelt island to ween her mother off the respirator system the hospital had basically forced on her and refused to take her off of…
the day comes for the transfer, the nursing home section “snatched” my in-law, and with “the peg”, claimed capacity to control her care…when we protested, they claimed that her medicare did not in fact cover all the care she had been receiving and handed over a bill for over 700 grand, payable if my ex wanted her mother back…
having been born on walpurgis but finding evil boring, I was delighted to have the opportunity to bitch slap evil wannabeez…so…
the magic, at least back then (2001) was that the billing codes would be sent before the procedure codes were entered…which is sorta kinda fraud, but fake news, as every large player did it, and no one cared as long as they were within a “range” of acceptable payouts…
so…while my ex was curled up in a ball in the corner sobbing, I walked into the medical directors office and described to him how many layoffs he would have to announce with my potential qui tam action…no no no sir, not just my in-laws billing, the entire hospitals regular billing practices…all 600 plus beds…and that regular policy of having staff tell illegals in spanish to use a different name this time so that they can get reimbursed, while I watched at the same time, in the same emergency room, americans being denied care because of lack of insurance…since they were structured as a non-profit, there are certain irs rules that many are not familiar with in respects to public availability of financial records…needless to say, they brought in lawyers and some former fed guy with a joke PI badge, imagining that they would blah blah blah me for having the audacity…
which only allowed my cheshire cat smile to blossom…
I calmly reminded them that they also had raised funds with special municipal bond type funding with SEC filings and had not disclosed the risks to their manner of billing and the risk to continued operations…
and also pointed out, since they had not mentioned they had made billing errors up until the moment they snatched her, it might not play out too well describing my ex in law being held hostage…
might be hard to fill in those nice little brand spanking new beds in that nursing home if it was on page 4 of the new york post that they were filling the beds by kidnapping…
sadly, after they handed back my in law, she felt so good after three days at the new facility on Roosevelt Island, she did not pay attention to the warning about her enlarged heart and literally talked herself to death at the facility…
biffland…america is caught in a bad groundhog day type loop of biff being the big boss in back to the future…
thanks for sharing that and good on you for pushing back.
I knew someone that worked as a medical coder. As you’d expect, there is enormous pressure to code quickly, which may entail deciphering physician’s notes and then deducing the “proper” codes. It sounds like a miserable job, to be sure.
Coding not just for accounting and accounting fraud … but micromanagement by Big Data on the medical side, not just ancient epidemiology, but every detail on cancers etc. That is why ICD-10 is so much larger than ICD-9. And Medicare drove this .. the Medicare folks decide what is or is not a code, on an annual basis. So … don’t expect Medicare-for-all to fix this.
What I mean by Medicare-for-all is you should just go in and get whatever you need. The patient should not have to handle any codes, bills, paperwork, or anything else. Free health care. If you want an optional procedure, and it’s denied, OK. But no paperwork.
To quibble an otherwise excellent post, the term ‘phishing equilibrium’. I get the spelling of phishing, to show an intent to fraud by digital means. But I question the word ‘equilibrium’. The phenomenon looks more like a occurence rather than a balancing point (equilibrium). How about ‘phishing opportunity’?
Lambert is picking up on the usage of George Akerlof and Robert Schiller in Phishing for Phools: The Economics of Manipulation and Deception. Had you bothered searching on the site or generally, you would find they defined “phishing equilibrium” on the first page of their book.
Apologies for my misunderstanding.
Medical coding could kill you.
My GP says we do not look for problems when asked about an issue.
I did get sent to a specialist as a family member had thalassemia minor I had forgotten to list.
I went to the blood specialist but they could only run tests and look for the thalassemia and could not test for the iron issue that started the process, no code.
Please, a little modest proposal.
I believe you could go to a specialist with a code for a condition and be dying in the office because of another issue not coded and they would be required by the system to say we do not address that problem. Please go down stairs or call 911. An exaggeration I hope to make a point.
Medicine is lost.
Patients march through the door.
Five minutes to code for billing.
The caregiver is worn stretched like ruts in a dirt road.
It is humanly warring for one and so hopefully personal for another.
Thank you Lambert. One can only wish that some decision makers would read what you write. Single payer is not going to help as long as providers to include hospitals and doctors are not put on fixed income or salary. If one compensates based on a metric the people getting the compensation will game to the metric. You get what you pay for. The current crop of electronic medical records, for example, are designed to maximize coding and have little or nothing to do with patient care. We are paying for upcoding and the computers encourage it by automatically putting in stuff that is not pertinent to the problem…..and was probably not examined. I saw a patient the other day who said they saw a neurosurgeon and I looked at the computerized note and it had all the reflexes and exam points in it. I saw something way different on exam. I asked the patient, “did he examine you? Did he touch you?…..the patient’s answer……no…..he just looked at the MRI scan and mumbled something. Of course, on the other hand, we see a lot of patients that claim the doctor did not examine them and they were examined and we ask…..what do you mean? and the answer is the doctor did not get an MRI scan…..even though it was not indicated. I am seeing, even in places with salaried doctors, unnecessary and inappropriate surgeries done when management makes it clear that OR utilization is a metric that will be used to determine whether the doctor will have a job next year. Surgeries are designed to maximize coding. The way procedures are done is based to a significant degree on coding. For example, a laminectomy without magnification pays significantly less than one with magnification. Guess what……everyone uses a microscope in back surgery (certainly unnecessary in the vast majority of case and not helpful in many meaning leading to worse surgery)…….some just wheel it in and look through it and wheel it out……Ding!!! Utilization drives funding in a centrally controlled system. If patient satisfaction is used as a metric the results are equally bad. Patients want surgery for a lot of reasons often unrelated to any surgical problem…..disability claims, compensation, mental, work excuse…….you name it. And patients often are convinced one thing is the problem when it is something else. The only solution is to put all doctors on salary, eliminate virtually all patient satisfaction metrics, eliminate all production incentives and let the doctors determine who gets what treatment based on science and functional outcomes. When patients want surgery to objectify their disability claims as in the VA or worker’s comp the doctor can say no with no risk to his career or family. This is the major reason the VA is backed up by the way. Vets constantly bug the doctors for more treatment so they can bump up their VA disability and the strategy works. The doctors know that if they don’t give them what they want they will get a negative rating and if you get a few your are gone. The rule at the VA is give the patients whatever they want. What do we think the narcotic epidemic is about? Why do so many VA doctors hate their job? We can afford to put all doctors on non production based salary. I read in the New York Times yesterday that firefighter paramedics in California are commonly making 200 to 300K per year with overtime. I have some firemen/paramedics in my family and they are doing that well (they are in Ca) and the medical training is minimal. A lot of the overtime is sitting around the firehouse working out with weights or watching videos. The firemen overtime is a lot of being on call time except they are paid. They sleep over in the firehouse and are paid. The doctor sleeps at home on call and he is not paid. I know many doctors that would love to make what they make, especially along with their pension, and they have spent decades in training and they work as many hours as my paramedic relatives and take a lot more hours on call. One of my relatives could have gone to med school after college and decided to be a fireman/paramedic instead. Not a bad decision from my standpoint. He is doing better than the ER doctor who has to take the patient over when they get to the hospital and way better than the primary care doctor who has to take care of the patient later. Same or more income and a lot less stress and liability and a lot more time off and all with three months paramedic training and a lot of political pull to get the job. He is going to be retired with a pension in ten years or so after ten years so far on the job and the pension is going to pay him what he is making for life…..and he never has to look at a computerized medical record or think about ICD 10 or coding. If we can afford gold plated firefighter salaries we can afford reasonable doctor salaries and pensions nationally (perhaps with an upscale to serve in underserved areas and a downscale to serve on the California coast.) So as long as we have pay for production on the provider side and pay for patient satisfaction on the patient side you are going to have an explosion in procedures, complications and costs and terrible outcomes even with Medicare for all. Money and medical care mediated by rent seekers (the insurance industry) in an environment with a gross surplus of providers (another issue entirely with similiar causes) is a really bad mix.
Thanks for this terrific comment, especially the part on salaries. I take the point.
My friend also had a horror story on MRI, where it was clear, after they ran a second MRI that the first people had either not run it properly — it was an MRI mill using obsolete machinery — or had misinterpreted it.
So they didn’t have cancer after all! (Needless to say, a bad moment.)
Makes you wonder, in fact, whether — slipping into Archdruid mode here — we need the coding at all. Does the coding demonstrably improve health care outcomes? If not, why are we doing it? Wait, don’t answer that…
I was thinking the same thing. If doctors became salaried civilian employees of the government the whole complex code thing theoretically goes away, certainly the abuse goes away, or at least is considered outright corruption and is dealt with legally.
I would think I would think the HMOs would be the best example for efficient billing procedures since end to end the process is internal so at every step the company has an interest in proper documentation and low costs.
Interesting interview with an activist/MD re the NHS and neoliberalism just posted by TheRealNews network.
https://www.youtube.com/watch?v=TsoZeg6CDRY
While I support single payer, I seriously doubt that ICD-10 will go away. So while the patient doesn’t have to waste time on billing disputes, errors may still occur intentionally for fraud (maximization of profit) or unintentionally out of ignorance or even improper diagnosis or improper procedure. So a coding error may still exist in your medical record that may affect your future medical treatment. Furthermore, code review will still have to be performed to minimize fraud, improper diagnosis and/or procedure. This will be a cost that will have to be borne by the administration of single payer.
My sister-in-law is a code reviewer for insurance companies in the area of physical therapy (she has two PhD’s; one in PT & the other in something like special education administration; clearly over-educated). She told me that the number one error by far was improper procedure, usually done by a PT with less than 5 years experience. She will call the PT and advise on proper procedure (the reason why the claim is being rejected due to improper procedure) and recommend that the PT find a mentor to assist in furthering their practical application of procedure.