Yves here. The press and punditocracy regularly mentions that Americans pay more for drugs thanks to not having the government either negotiate or regulate prices.
This paper identifies another less well known aspect of health care crapification: the too-common use of dubious treatments and technologies.
I’ve mentioned before that over 85% of the “new drug applications” in the US are for minor reformulations, such as a timed-release dose so that a medication needs only to be taken once a day, as opposed to the previous once every eight hours. Not only does the so-called NDA extend patent life, but the reformulated drug is regularly sold at a large price premium to the older version.
When I lived in Australia, its Therapeutic Goods Administration would read the literature carefully on the medications that treated various ailments. They would choose the one or ones that were the most effective and would bargain hard on price. Often the drugs they selected were not the newest.
Similarly, many procedures that have become common in the US don’t appear to any benefit. I’ve been leery of orthopedists since 1992 (I will not bore you as to why). Four studies have founds that four common orthopedic surgeries produce results no better than a sham surgery. Yet many patients still haven’t gotten the memo. An older man in one of the gyms I frequented, who was dutifully working out despite not appearing to get much benefit, had a regimen that included what I recognized as knee rehab exercises. I would chat him up occasionally. One time he remarked almost proudly, as if this was proof he was doing a good job of personal maintenance: “I go in to see my doctor ever three or four years and he cleans my knees up.” I didn’t have the heart to tell him that wasn’t helping and could even over time make things worse.
By Margaret Kyle, Professor of Economics and Chair in Markets for Technology and Intellectual Property, MINES ParisTech and Heidi Williams, Class of 1957 Career Development Associate Professor, MIT Department of Economics. Originally published at VoxEU
Despite higher per capita healthcare spending, US health outcomes compare poorly with other developed nations. One potential reason is that the US healthcare system creates incentives that promote the faster adoption of medical technologies with minimal benefits. This column tests this claim using data on the quality and diffusion of new pharmaceuticals in the US and four other countries. The results suggest that compared to Australia, Canada, Switzerland, and the UK, low-quality drugs diffuse more quickly in the US relative to high-quality drugs.
Although the US spends more on healthcare per capita than any other developed country, it does not enjoy better health outcomes. Are institutional features of the US healthcare system driving this apparent inefficiency? Garber and Skinner (2008) hypothesised that the fee-for-service system of reimbursement prevalent in the US may create incentives for faster adoption of new medical technologies that may have minimal clinical benefits. However, directly testing this hypothesis is generally complicated in part because it is difficult to construct consistent measures of healthcare utilisation across countries in a way that holds quality of care constant. For example, a surgical procedure may be used more in one country than another because the quality of the procedure is higher in that country, not because it is inefficiently administered.
In a recent paper, we argue that the adoption and diffusion of new pharmaceuticals across countries is well-suited for testing the Garber-Skinner conjecture (Kyle and Williams, 2017). First, we can be confident that pharmaceutical use is relatively consistently measured across countries – there is little difference between the cancer drug Avastin sold in the US and the cancer drug Avastin sold in other countries. Second, for pharmaceuticals it is possible to exploit an existing measure of drug quality that is based solely on clinical value (that is, this quality measure is independent of the drug’s price). Despite having some limitations, this quality measure allows us to compare whether the US differs from other developed countries in the adoption and diffusion of drugs with relatively high therapeutic value relative to those that provide more marginal gains.
Data and measures
We analyse quarterly data from 2000-2013 on revenues and quantities sold for new pharmaceuticals in Australia, Canada, Switzerland, and the UK provided by QuintilesIMS Health. We aggregate across all packages or presentations of a drug to the molecule (or molecule combination) level.
For our measure of drug quality, we rely on assessments of France’s Haute Autorité de Sante (HAS). When a drug is introduced in France, the HAS evaluates both its clinical importance and its relative therapeutic value over existing treatments. The latter, referred to as the ASMR (amélioration du service médical rendu, or improvement in actual benefit), is a score from I to V. ASMR I corresponds to major improvements. Gleevec, generally considered a breakthrough treatment for some cancers, is an example. ASMR V is assigned to all generic drugs (which offer no clinical benefit relative to the originator version) as well as other new drugs with no evidence of clinical superiority over existing treatments. The ASMR evaluation takes place before price negotiations in France – it is an assessment of clinical value, not an assessment of cost-effectiveness.1
Our sample is confined to drugs for which an ASMR rating is available and for which we have complete sales data from the time of launch. In addition, we focus on new brand-name or originator products – that is, new molecular or biologic entities – rather than generic drugs. We focus on comparing outcomes in the US to outcomes in four other major developed countries: Australia, Canada, Switzerland, and the UK.2
Results
Our key research question is: how do higher- and lower-quality drugs diffuse over time in the US relative to our comparison countries? We measure diffusion by sales of standard units (that is, by measuring quantities rather than revenues), and focus our quality metric on a comparison of more (ASMR I/II/III) and less (ASMR IV/V) therapeutically valuable drugs. We analyse diffusion over the first six years after a product is launched, during which time a new product should generally not face any generic competition. We estimate a regression specification that pools all five countries and includes fixed effects for drugs, countries, and years since launch.
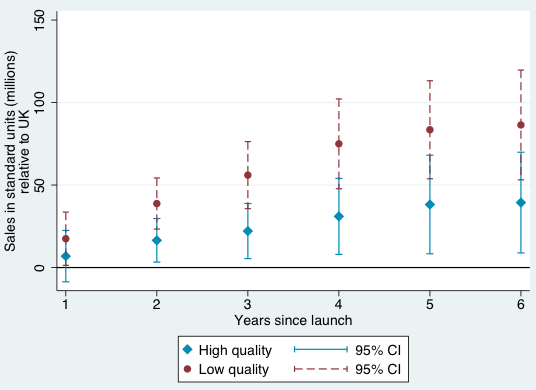
Our results suggest that – consistent with the Garber-Skinner conjecture – the US is indeed “uniquely inefficient” in the sense that low-quality drugs diffuse more quickly compared to high-quality drugs, relative to the comparison countries we analyse. The same pattern holds if we compare the US against each of our comparison countries individually, although the difference in coefficients is only statistically significant in pairwise comparisons when comparing the US to the UK and to Switzerland. All of these results are strengthened if we omit the ASMR III (‘intermediate’) quality category.
Figures 1-4 provide a graphical summary of our results. In each, we plot the diffusion curves – units sold relative to the initial year of launch in each country – for lower-quality drugs (in dark red) and higher-quality drugs (in light blue), with 95% confidence intervals. While the confidence intervals for low and high quality drugs are overlapping in this more disaggregated comparison, qualitatively the overall patterns are remarkably consistent – with the exception of the year of and first year after launch in Australia and Canada, lower-quality drugs consistently diffuse more in the US relative to higher-quality drugs, judged relative to any of the four comparison countries.
Figure 1 Diffusion, US and Australia
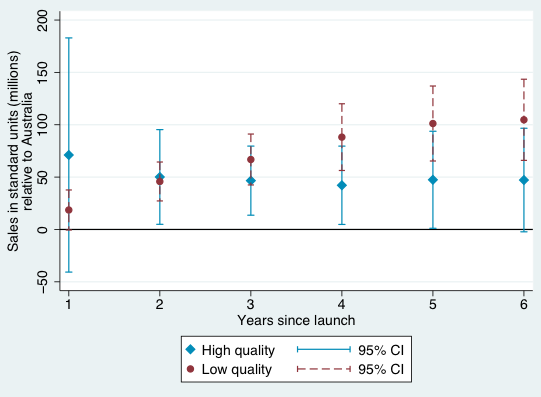
Figure 2 Diffusion, US and Canada
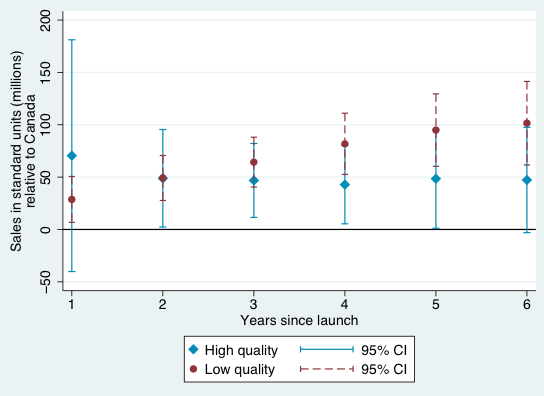
Figure 3 Diffusion, US and Switzerland
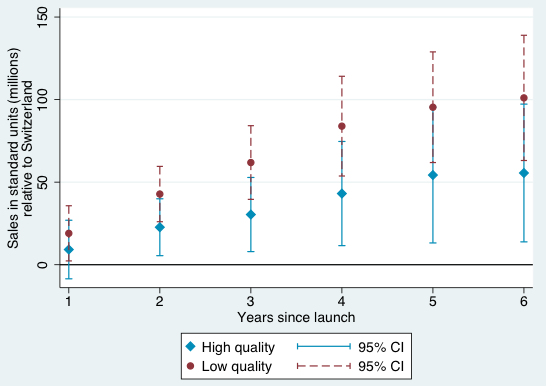
Figure 4 Diffusion, US and UK
Conclusion
Prior work (Kyle 2007, Kyle and Qian 2014, and Cockburn et al. 2016) has attempted to quantify the influence of factors such as intellectual property rights and price control policies on firms’ decisions to launch new drugs globally. To the best of our knowledge, our paper is the first to focus on how diffusion varies across countries based on a measure of therapeutic quality. While our drug quality measure is of course imperfect – in particular, while it is independent of price, assignment of these measures happens in the shadow of price negotiations – it arguably takes a step forward in understanding the welfare implications of cross-country differences in drug diffusion.
Our tabulations suggest that low-quality drugs diffuse more quickly compared to high quality drugs in the US relative to these four comparison countries. These patterns are consistent with the assertion in Gruber and Skinner (2008) that the US healthcare system may be “uniquely inefficient” in the sense of fuelling the rapid adoption and diffusion of medical technologies with small or unknown benefits.
Our hope is that, in the future, the newly linked data developed in our paper can be combined with an analysis of policy changes in order to analyse the potential roles of specific factors in explaining the higher diffusion of lower quality drugs in the US relative to other countries. For example, does the use of centralised health technology assessments in countries outside the US encourage the adoption of technologies with higher measured benefits? What are the longer-term consequences of such policies, not only for health spending but also for health outcomes?
See original post for references


Crapification.
Like appliances, furniture, clothes, and sooo much more!
drugs and medical care generally in the US of Goldman Sachs is junk.
Heck, if I didn’t research my own symptoms, specify the tests, read the labs and imaging, check for drug interactions and triple check the insurers and physician groups for prior authorizations…nothing would even happen.
I’m not sure what doctors even do anymore,,,except collect $300 every time I walk in the door.
I do know what those vacant-looking besuited young “professionals” wheeling their luggage around hospitals do…bribe “doctors” to peddle more of their overpriced drugs.
I’m thinking of DIY dentistry next.
Hi Cripes. You said “I’m thinking of DIY dentistry next”. I have doing “oil pulling” for the last week, and it has been a miraculous eye opener in my N=1, ongoing case study (I am the only subject).
“Oil pulling, also known as “kavala” or “gundusha,” is an ancient Ayurvedic dental technique that involves swishing a tablespoon of coconut oil in your mouth on an empty stomach for around 20 minutes. This action draws out toxins in your body, primarily to improve oral health but also to improve your overall health”.
I have been using a heaped tablespoon of coconut oil, first thing in the morning and last thing before bed. I swish for 20 minutes and spit outside on the ground. My teeth and mouth feel like I have just had my teeth cleaned (only better). AND, I feel healthier and happier! Supposedly, if your mouth is healthy, then everything downstream is healthier. Anyway, my tongue is pink now, instead of white.
I love the ancient, multicultural goofiness of “Kavala”.. It is a low risk, high reward activity.
The USA Pharmaceutical Industry- In my mind, right up there with “famine, plague, war, and drought”. Lord, why have we been cursed by these creatures? What have we done????
How do you have a “heaped” spoon of what appears to be a liquid?
The melting point of coconut oil is somewhere around 75 degrees Fahrenheit. It can be a solid at a moderate temperature.
Surface tension.
It is more subtle than bribes. One of the first pieces of paper given to patients at most health facilities is the HIPA (privacy) form. When you sign it, one would believe it protects your privacy! Instead it gives everyone, except you, access to your medical history including prescription drugs. The pill peddlers peruse the records to see if you are faithfully dosing and refilling. If one is getting prescription drugs through Medicare, you get a text or email reminder from the drug company reminding you of your unfaithfulness. During a recent visit to my primary doctor, I see a notice on the sign in station window and in the exam room: Bring All You Prescription In Their Bottles At Each Visit……in other words, I am falling behind on my points for a free trip to Hawaii and I need to check up on your faithfulness to swallow the pills not your health!!
Think about this in terms of advertising and the role of information in guiding treatment. If you’re sick, isn’t it the doctor’s job to know what the cheapest, best treatment is for your condition?
Why advertise your drug if it’s the cheapest and best? Isn’t the doctor supposed to know right off the bat to use it? If this isn’t the doctor’s job, then why do we even need these pad-scribbling monkeys?
You can’t have this both ways. You can’t say doctors are qualified to dispense medicine/medical advice and then turn around and claim there’s some magical benefit to “advertising.” There isn’t. From a rational investment perspective, companies should only have to market their drug if #1 it’s so new that nobody knows about it or #2 it’s so bad that nobody would use it except those susceptible to marketing/gullible enough. #1 only really works for an audience of doctors so that pretty much leaves #2 or an arms-racing scenario where people clamor to get their brand out over the background noise.
To give you some idea of how big a disaster Madison Avenue marketing has been for medicine, I’m allergic to every over-the-counter allergy pill on the market. They love colorful little, sweet-tasting pills. As such, they all have fillers or food dyes I can’t tolerate. Aside from the obvious allergens like maltodextrin and rice, these pills often contain sugars that stoke the very immune cells directing the response to allergens.
It gets worse.
Broad-spectrum antibiotics kill friendly flora in the gut, leading to colossal c. diff infections. Opiates produce chronic pain when they lead to addiction (Perdue). NSAIDs like Celebrex caused the very arthritis conditions they’re sold to treat (both osteoarthritis by inhibiting stem cell repairs and rheumatoid arthritis by inhibiting regulatory T-cells – which they’re so good at, they’re used in chemotherapy regimes to induce autoimmune attacks on tumors).
In the words of Nobel Laureate, Angus Deaton, we have “iatrogenic medicine” – medicine which causes the very diseases its sold to treat. We have what Washington excels at, another self-licking ice cream cone. It’s the kind of game rent-seeking oligarchs love and the only way out of it is to never play it. The first move is deadly and expensive. You only find this out when you read the medical literature yourself for a few years. It is a classic agent-loss/fraud problem.
The privatization of public goods leads to extortion for profit. Military contractors don’t win wars because it puts them out of business. For-profit prisons don’t rehabilitate criminals or invest in crime prevention because it empties their beds. Healthy patients aren’t repeat customers. If you treat patients with something cheap and effective, they never come back. The goal is profit, not health.
Private security contractors want national insecurity. It drives up demand for their services. Private, for-profit education wants more ignorance and higher course prices. Any monopoly making a profit on public goods will seek to raise the price by decreasing supply (of actual effective medicine, in this case) or driving up demand (by creating sickness or suppressing wellness).
+1,000,000. Thank you!!
I’d read this as: applying the profit motive to health care produces uniquely bad outcomes. This is just one example; there are many others. How many examples do we need to conclude this is a failing system, eating its own tail?
or should it be:
“applying the profit motive produces bad outcomes?”
If customers, the public, are personal to the business and business owner, then the customers will probably be treated well.
If customer are impersonal, as they are for most large businesses, I believe then trend is treat them as marks or suckers.
Which modifies the assertion above to:
“impersonal customer relationships applying the profit motive produces bad outcomes.”
Consider Oil Companies, Airlines, Banks, large retail chains, etc all of which have impersonal relationships with customers, and a unique example, the railraod companies which were the first large companies, had a reputation of being indifferent to customers, and were demolished by the US Highway system, to the delight (as I understand) of the populace.
Large companies, just because they are large, have impersonal relationships with customers.
Good point. I think I was using unique in the sense that, when these outcomes manifest in the healthcare system, people die. Dr. Dao got his teeth knocked out because of the large corporate culture of indifference to the customers, but at least the airline didn’t kill him.
All the more reason to avoid the American “health care” system.
How do you accomplish that?
Not a choice for millions. Simply can’t afford to participate. Must be weird to be in a public place and listen to others complaining. Maybe there is an upside in that people never have to worry about getting a doc, paying for prescriptions or planning for end of life care.
The Whole thing is mostly an excercise to ****er the peasants for a fast buck, and then pretend that medical “care” was done; why is anybody surprised at the outcome?
See “Medical Nemesis” by Ivan Illich. Written in the 70’s and still completely relevant.
Yves, Your comments regarding many orthopedic procedures are right on. What you have to remember is that the majority of patients that go to orthopedic surgeons are litigating. Very few people slip and fall without some sort of fault….be it a slippery floor at McDs or stairs or worker`s comp. Even if it is a pre-existing condition the usual comment is that “it did not bother me before” so we have a “lighting up” of a pre-existing condition that but for the job would never have been noticed or come to medical treatment. When no surgery is done the insurance industry is just not willing to pay very much. A MIST (minimal injury/soft tissue) back might be worth 30K but if you can get screws put in and a spine fusion it can be 550K or even a million….and for that kind of money patients will lie down on the table for just about anything. An unoperated back in the VA/military might be worth 10% and a spine fusion will generally give you a medical board and a 100% life pension with full medical care and benefits to include often free tuition for your kids, no state or real estate taxes etc. And being disabled for the back is socially acceptable unlike psychiatric conditions, for example. You can still go out and fish and hang out with your peers.
In this economy that is a pretty good deal for a poorly educated worker in his mid 30`s. So you might ocnsider that the outcome from orthopedic surgeries might be pretty good for the lawyers and patients in one sense and the surgeons……for society not so much……depends how you measure outcome.
I’ve written before about a town called Vernon, FL, where not so long ago the residents, some of them, would maim themselves to get a nice insurance payout. http://mentalfloss.com/article/67097/nub-city-vernon-floridas-decade-long-insurance-scam
Now we have welfare by disability, or too often “just die” after the looter locusts have stripped a place and flown on to the next green patch.
Sorry, I have to differ with you. This is not about poor people. This is how orthopedists operate, pun intended. I saw an orthopedist who is supposedly the second best knee guy in NYC (which = football players + rich people) who was all gung ho to operate on an ambiguous MRI: “I’ll just go in, have a look, clean it up.” He basically said he was going to go on a fishing expedition in my knee. I got a second radiological opinion (from an entire team at Cedars Sinai) and they said “Your knee looks perfectly normal”.
Similarly, the guy in my gym who has been trained to have his knee messed with every few years was at an upscale facility. My trainer, who rehabs pro athletes, has tons of similar stories.
I can relate because I had a similar experience. These very abundant type of orthopedists should be a disgrace to the medical profession. On the consumption side there seems to be a surgery banalization by every time larger societal groups. It is not just the celebrity exhibiting on TV her annual cosmetic surgery along with her yearly vacation trip. My best friend told me “nowadays the only surgery that seems to skip a beat is the necessary to avert death”. A bit of an overstatement but not too off.
Just a minor point, Yves. You specifically mentioned “time-released” in the category of “minor reformulation” of a drug, and I wanted to point out that at least some time-released formulations have very specific benefit beyond convenience. In my case, I use a time-released version of morphine to treat a lingering consequence of a surgery where the regular dosage simply does not work. More than that however, I’ve read in chatrooms on my drug that the street value of my formulation is far below the value of the regular formulation, so I suspect (and my own experiences largely confirm) that the addictive capacity of time-released morphine is significantly less than regular morphine, And in the two cases my insurer (!!!) has tried to change me over, my protest included just this point.
In fact, I strongly recommend that the two versions of morphine be tested for just this possibility. Can you imagine if we could clear up a good portion of our opiate problem simply by having doctors change over to prescribing the time released formulation?
Interesting point. However, the specific example of time release reformulation I was told about years ago was Wellbutrin, as an example that the reformulations are for patient convenience and not a serious medical purpose.
For stuff like Oxycontin, the drug in it is just as addictive. It’s the same exact drug, but one of the main features of the time release is that you can’t shoot it up, or snort it in many cases. Guaranteed that addicts will find the ones that they can shoot up, or just switch to heroin.
I love the intro by Yves!
Thank you Yves.
Can count on one hand how many pills I have taken in last five years.
Lost my trust with docs years ago. There is only one person I trust to look after my health, through prevention and avoidance, me…
My father recently received a corticosteroid shot for his knee. It did absolutely nothing (which a recent review of the evidence just confirmed). I gave him DMSO and the next day his limp was gone.
My first brush with orthopedists came in high school when I had two “lateral releases” for my knees (turns out the problems were G.I. and autoimmune). After I found out how deadly the Feldene was that he sent me home with, I started thinking I never needed the surgery – which a physical therapist confirmed years later. I got so angry, I went out and joined the college swim team. It was the only thing that made my knees feel any better and I swore I would never go to another orthopedist. It was the best medical care I received for the first thirty years of my life.
If not for my surgeons I’d be dead or paralyzed. Without time release morphine I am more disabled by pain. As it is every move is painful.
If pot found in Piss,no morphine.
Doctors first of the wage slaves, so they don’t lead the system.
Depression is pathology, anger is not.