Lambert: I have severe priors on ADHD, and know little of asthma. Readers, do any of you have experience with these issues, whether as patients or practitioners? (Presumably, the VoxEU headline, which I retained, means the diagnosis of these conditions, not the conditions themselves.)
By Anna Chorniy, Postdoctoral Research Associate, Center for Health and Wellbeing, Princeton University, Janet Currie, Henry Putnam Professor of Economics and Public Affairs and Director of the Center for Health and Well Being, Princeton University, and Lyudmyla Sonchak, Assistant Professor of Economics, SUNY Oswego. Originally published at VoxEU.
Diagnoses of asthma and ADHD among children in the US have increased over recent years. This column argues that one contributor to this increase has been a change in Medicaid from a fee-for-service model to a managed care model. This change created incentives that reward higher diagnosis and prescription rates, while not necessarily improving health outcomes.
In the last decade, the number of US children diagnosed with asthma and attention-deficit/hyperactivity disorder (ADHD) has inexplicably been on the rise. ADHD is a neurological condition defined by persistent symptoms of inattention and/or hyperactivity-impulsivity. It is one of the most common mental health disorders affecting school-aged children. Asthma is a chronic inflammation of the airways in the lungs. It is one of the most common physical chronic childhood illnesses, and the most frequent cause of childhood emergency room (ER) visits and hospitalisations. The number of children whose parents reported that they had ever been diagnosed with ADHD increased by two million between the 2003 and 2011 waves of the National Survey of Children’s Health, rising to 11% of all school-aged children (Visser et al. 2014). Between 2001 and 2010, the number of children who had been diagnosed with asthma increased from 8.7 to 9.3%, although the number who reported an asthma attack in the past month held steady and the number of asthma-related hospitalisations and deaths continued to fall (CDC 2012).
While the increase in asthma has been described as a “mystery” (CDC 2011), researchers have found that the increase in ADHD caseloads can, in part, be explained by school accountability pressures and special education financing incentives. For example, Bokhari and Schneider (2011) look at the effect of the school accountability laws on medical diagnoses and subsequent treatment options of school-aged children. They use variation across states and over time in specific provisions of the accountability laws and find that accountability pressures matter. Children in states with more stringent accountability laws are more likely to be diagnosed with ADHD and consequently prescribed psychostimulant drugs for controlling the symptoms. Morrill (2017) looks at the differences in special education financing policies across states and finds that children living in states where schools receive more funding for educating students with disabilities are 15% more likely to report having ADHD and 22% more likely to be taking medication for ADHD.
While school-level incentives clearly matter, ADHD diagnoses have been rising even in states, like South Carolina, without any changes in such incentives, and rates of other chronic conditions such as asthma are also rising. Increasing rates of chronic conditions among children are a grave concern, and also a puzzle given that other health indicators such as mortality have shown great improvement, and underlying causes, such as smoking and pollution, have been declining (Currie and Schwandt 2016).
In a new paper, we propose a novel hypothesis, which is that the increase in diagnoses for both ADHD and asthma was driven at least partially by changes in Medicaid, the means-tested public health insurance programme that covers low- to moderate-income children (Chorniy et al. 2017). In national data, the increase in treatment for ADHD and asthma over the course of the 2000s was largely accounted for by children on Medicaid, and not by children with private health insurance coverage. Figure 1 shows that while the overall number of children taking any kind of prescription drug fell, the fraction with prescriptions for ADHD medications rose, and all of the increase is accounted for by children on Medicaid. Figure 2 shows that the fraction of children taking prescription drugs for asthma has also increased. Up to 2009, it increased at a similar rate for the privately and publicly insured, while after 2009 all of the increase has been among Medicaid recipients.
One of the largest changes in Medicaid over the course of the 2000s is that it was converted from a largely ‘fee-for-service’ programme, in which physicians were reimbursed for each service provided, to a managed care model in which providers received a capitated fee intended to cover all services provided to a covered child. Nearly 80% of states had transitioned their Medicaid programmes to managed care by 2016.
Figure 1 Nationwide trends in filled ADHD prescriptions
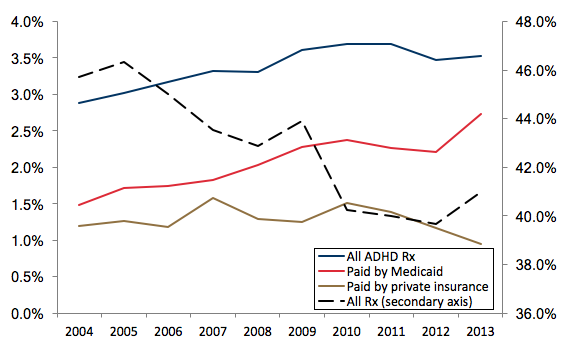
Note: The sample includes all ADHD prescriptions filled by children under 17 years old.
Data source: Medical Expenditures Panel Survey (MEPS), 2004-2013.
Using Medicaid claims from South Carolina, we show that the shift to managed care contributed to the increase in asthma and ADHD caseloads through three mechanisms (Chorniy et al. 2017). First, managed care improved access to most forms of care (though the use of specialists fell). Second, capitated payments to managed plans are ‘risk adjusted’ so that insurance plans receive higher payments for patients who are thought likely to generate higher expenses. In South Carolina, plans receive higher payments if children fill a prescription for one of the listed chronic conditions, which includes asthma and ADHD. Hence, the risk-adjustment mechanism creates an incentive to write at least one prescription for a condition with an added weight, although there is little direct incentive to ensure follow through on medication compliance. Third, managed care plans are evaluated on how well they deliver recommended screenings for children, and other things being equal, would be expected to yield more cases.
These features of managed care plans may be particularly likely to generate increases in ADHD and asthma caseloads. Both conditions are common, so that additional screenings would be likely to turn up more cases. They are also difficult to definitively diagnose, but are nevertheless likely to be diagnosed and treated by family physicians rather than specialists. And for both asthma and ADHD, the frontline treatments are medication. Thus, diagnosing either ADHD or asthma will increase a plan’s capitated payment without necessarily increasing the cost of caring for a child significantly.
Figure 2 Nationwide trends in filled asthma prescriptions
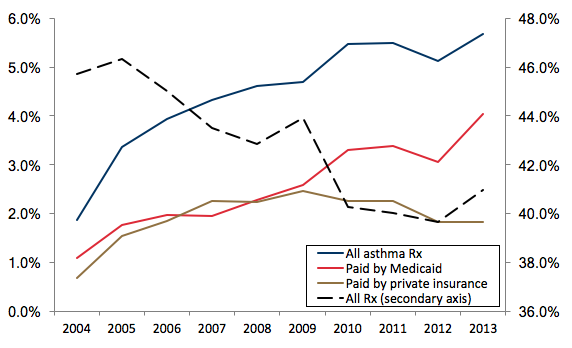
Note: The sample includes all asthma prescriptions filled by children under 17 years old.
Data source: Medical Expenditures Panel Survey (MEPS), 2004-2013.
The estimates suggest that all of these forces are at work. The switch to managed care in South Carolina increased the probability that a child on Medicaid received a well-child visit by 49.0%, and there were increases in the probability of having blood work, developmental and hearing screens, and vaccinations. There was also a 58% increase in the child’s individual risk-adjustment weight, with a third of the increase being accounted for by increased prescribing for asthma and ADHD alone.
The actual increase in ADHD and asthma caseloads in the Medicaid population over the sample period was 30.4% and 36.4%, respectively. The switch to managed care increased caseloads for these two conditions by 26.6% (ADHD) and 29.9% (asthma). An upper bound on the effect of increased screening alone is 15.7% (ADHD) and 18.2% (asthma). Hence, the switch to managed care accounts for the majority of the increase in diagnoses of these two conditions in this population over this period, and an increase in screening alone cannot account for all of the increase.
In principle, increases in diagnoses and treatment should improve health outcomes. Unfortunately, there is little evidence that this is the case. Instead, there were increases in preventable hospitalisations and in almost all types of ER visits. A large part of the increase in ER visits was driven by asthma, and over 40% of children with asthma received fewer than two prescriptions for asthma in the past 12 months, a proportion that remained constant with the advent of managed care. The only category of care that showed a decrease was office visits to specialists.
While managed care plans improved access to primary care physicians and helped to ensure that a larger share of children on Medicaid benefitted from preventive care, other features of the programme apparently backfired. First, risk-adjustment incentives distorted prescribing practices in that more children received at least one prescription medication, but providers had no incentive to follow-up on adherence.
Second, access to primary care and specialists seems to have changed in a way that encouraged reliance on emergency rooms even for non-urgent care. The large and striking changes in patterns of utilisation may or may not reflect deterioration in underlying child health, but they are certainly not consistent with improvements in the efficiency of the care provided under the Medicaid programme. They suggest that patients in Medicaid managed care may have experienced difficulties accessing primary care outside of the annual well-child visit that managed care plans are mandated to provide.
Children on Medicaid are among the most vulnerable patient populations. The evidence indicates that their care is very sensitive to the incentives provided by the reimbursement system facing insurers. Moreover, because Medicaid covers approximately 40% of US children, trends in diagnoses in this population are potentially large enough to help explain the mystery of climbing national rates of common childhood chronic conditions at a time when other child health indicators are improving.
References in original post.


Anecdotes are not data but both my sister and a close friend needed IVF, having children late (happening more often these days) and 3 out of their 4 kids are “on the spectrum” (not necessarily ADHD though one borders on it with a similar diagnosis). I just wonder if IVF and the “egg quality issue” raised on NC recently may have contributed to some of this increase in recent years? Just a hypothesis but think it deserves more investigation.
Furthermore quantifying health-related quality of life in kids is notoriously difficult – having being involved in the “valuation study” to obtain scoring for a Kids’ instrument – the CHU-9D – (and providing some informal input on at least one other) I know that significant numbers of children can’t do the task (thus compromising the representativeness of the “children population scores” but there is evidence that adolescents value mental health impairments as being “worse” than their parents do, suggesting the effectiveness of mental health interventions among kids may be understated in single payer schemes if “adult scoring” is used as a proxy.
Interesting theory. A friend of mine, whose youngest was diagnosed ADHD, had her two children (especially the youngest) very late in her childbearing life after unsuccessful IVF. So she doesn’t meet the IVF criteria, but the egg quality issue, due to the mother’s age, may have many ramifications that haven’t been studied yet.
Sperm quality, too, assuming the father is as old as the mother. However, I think that’s significant later, because sperm are made constantly while eggs age.
.
Not true. Eggs are continually made from stem cells.
Leaving both anecdotes and data aside, there is a principle in play here that I think is hard to discount. Given a list of things that can be billed for, a ‘medical business’ with an eye on profit is going to bill for them; and if those things are not found (in the proper, legally defined form) in the wild, they will be produced, just like any other manufactured and marketable commodity. Thus we should not expect the ‘health outcomes’ for which we might hope, but we do find the economic outcomes that we should.
This is a nicely done study.
Medicaid is a horrible system for taking care of 40% of US children and should lead to a concentrated effort for single payer.
The main problem is that it is state funded and many states are in big financial trouble and also they can’t print their own currency.
“”In South Carolina, plans receive higher payments if children fill a prescription for one of the listed chronic conditions, which includes asthma and ADHD.””
Simply put, insurance companies shouldn’t be involved in these sorts of complicated decisions. These are social decisions that should be publicly funded for the best interest of the population not the best interest of an insurance company.
I’m afraid there may be a couple of major flaws with this study, related to failure to control for other variables.
(1) Asthma: The authors claim that air pollution has been declining, but this is based on a single quoted paper. What really matters for childhood asthma is proximity to air pollution – children that live next to major freeways, shipping ports and airports are at a greater risk of asthma, and there has been no decline in such traffic. Indeed, the rising wealth inequality may have resulted in more families living in such low-cost neighborhoods (low-cost because anyone with any money would move away to cleaner environments).
(2) ADHD: Here we have the confounding variable of pharmaceutical marketing pressure. ADHD medications are all basically derivatives of the amphetamine classes; in fact methamphetamine is sold as ‘Desoxyn’ for treatment of ‘difficult’ ADHD patients; Adderall is amphetamine, and Ritalin is an amphetamine analogue. The marketing pressure here is very similar to that for opiates in the United States, i.e. direct advertising to parents and rewards for doctors who prescribe more ADHD cases. Notably, ADHD wasn’t even recognized as a ‘disorder’ before the 1980s, but the correlation between the rise of amphetamine abuse and the rise of opiate abuse is significant; many adult meth addicts began as childhood ADHD cases who got their drugs from the pharmaceutical lobby. Since opiates are more likely to kill than amphetamines are, there’s been less high-profile public discussion of the meth/amphetamine addiction situation than there has for opiates.
These complicating variables don’t seem to have been adequately addressed in this study.
This:
“The main problem is that it is state funded and many states are in big financial trouble and also they can’t print their own currency.”
is not entirely true. South Carolina did not expand Medicaid and the proportion of $ received is the 4th highest in the nation based upon income. Going into 2018, South Carolina will receive $2.52 from the Federal Government for every $1.00 it funds Medicaid. For the $1 billion Medicaid budget it has, the Federal Government will kick in $2.52 billion in funding, the forth highest in the nation. https://www.kff.org/medicaid/state-indicator/federal-matching-rate-and-multiplier/?currentTimeframe=0&sortModel=%7B%22colId%22:%22FMAP%20Percentage%22,%22sort%22:%22desc%22%7D
I can’t comment on the US system, but I do know that asthma was historically very under-diagnosed in Britain and Ireland. I know this personally as I spent much of my childhood and early teens being treated for ‘chest infections’ when I really had exercise induced asthma – finally diagnosed at age 15 when I was brought to hospital barely able to breathe.
I was told many years later by a relative who is a specialist in medical prescribing practice that asthma is one of the most commonly misdiagnosed conditions – he told me that even years after it was recognised to be a fallacy that childhood wheezing was caused by bronchial infections many older doctors insisted on treating asthma attacks with antibiotics certainly well into the 1990’s and later (this was in Britain). So far as I know its still a matter of debate in Europe as to whether the significant increase in asthma rates over several decades is due to environmental impacts or is simply the result of better diagnosis.
Its probably not relevant to the figures in the article, but it should also be noted that the rate of asthma was notoriously common among professional athletes when the most common prescription for it was ephedrine (a stimulant).
You have to jump through so many hoops to get a stimulant controlled substance refilled {actually have the paper and bring it to the pharmacist and just hope your doctor writes out 3 months worth at a time) that I don’t find it at all surprising that kids on medicaid don’t get the script refilled.
Medicaid has become a wealth transfer system to the big players in the healthcare industry. Any actual patient benefit is a byproduct of this highly corrupt program. Most of those who call for Medicaid expansion don’t understand who the real beneficiaries are.
The NY Times just ran a a story four days ago on a similar phenomenon with skin cancer diagnosis/testing and Medicare: https://www.nytimes.com/2017/11/20/health/dermatology-skin-cancer.html.
I don’t need a bunch of Princeton eggheads (okay, and a token Oswego person) to tell me that any group of people who can game a system will always do so. The real question for me is why our so-called leaders would allow things to be set up this way, when they surely know what I know.
If we assume the increase is real, I’m going with pollution and our general chemical load as the cause. There is also solid evidence that kids are more likely to get asthma if they don’t play in the dirt. (Personal note: our neighborhood was being built when I was growing up, so we played in the dirt piles. My mother had us undress BEFORE we came inside, and sometimes hosed us down. Some allergies, but no asthma.) There’s a child-care book called “Let Them Eat Dirt.” Be careful which dirt, though; not too close to the house or to a highway.
As I assume Lambert is implying, it’s very questionable whether ADHD is a thing. An increase in diagnoses could reflect more rigid classroom practices, for instance. But the wonders of chemistry could be a factor there, too.
Increased rates of childhood asthma have been occurring in much of the world (especially rich countries) for several decades so I think attributing it to changes in the US healthcare system lack broader context.
ADHD overdiagnosis is a huge can of worms.
Going back to the big article on lead poisoning and crime awhile back, it’s still the case that many homes in suburbs and even rural areas still have lead-contaminated soil, and city lots are practically toxic waste dumps. It would be astounding if there weren’t large numbers of kids with neurological deficits. ADHD is an effect of many kinds of toxic poisonings, AND it’s genetically dominant, as well. Add in climate-change-induced levels of pollen and molds, and continuing exposure to pesticides in air, water and food.. many other disorders are on the rise as well. Gut problems are a biggie now. Data collection on all this is pretty bad in America, but looking around at people I know, remarkable amounts of autism, cancers, allergies to multiple foods, asthma, you name it, are now *common*. And this is a relatively wealthy area surrounded by much state forest. We’re all swimming in industrial toxins. My feeling is that there is still a great deal of underdiagnosis.
Every time I read one of these articles or studies (or think about my own biases re diagnostics) I can’t help but view them through my own professional experience. I work in tech and have spent a decade+ in the area of tech that requires keeping things up and running. Often I have to make quite a lot of assumptions pretty quickly, and usually I have to be able to explain my actions later in a reasoned way so that the rest of the team I work within can assist, or explain why something didn’t come back as fast or gracefully as possible, or whatever. There are a handful of explanations for any given situation that will be uniformly acceptable (hardware failure, provable upstream failure) and then there are things like a failure scenario the end user is already familiar with. Outside of those things I’m expected to come up with the solution or quickly pass it to someone who can. When that doesn’t happen there is a huge corporate kabuki that plays out, where the blame is shifted until financial compensation is reached to resolve the issue.
Obviously tech and medicine are quite different. They’re both financialized, though, so I can see the incentive to assigning a problem to a bucket even if it’s just a best guess; open questions lead to bigger losses by the party that can’t explain the problem to the consumer if there is an avenue for dispute that affects the cost.
Also, as a mid 30s millennial working in tech – almost everyone I work with who has discussed it has had an ADHD (and/or depression) diagnosis.
This is a very disturbing report, and it will take more than a single reading for me to unpack it.
First, there is global budgets and capitation vs fee for service. If only human greed was not such a dominant force in everything! M4A proposes that global budgets will promote cost control NOT at the expense of quality care. For this to be true, it seems, the incentives will need to be carefully thought through. M4A does propose to buffer docs from the profit motive by putting them on salary, and to pay primary care docs better to reduce the disparity with specialists.
Second, as a clinical social worker I can concur that Medicaid IS an awful system. In some counties around Chicago there are only a few providers who will accept it. And indeed, who wants to be stiffed for not just months but years by taking on the state of Illinois as a payer? That is the problem of letting the states, which are obviously not sovereign currency issuers and are mostly required by law to balance their budgets, administer a program like this.
Third, having provided home services to the children it serves, I can attest to the myriad environmental barriers to kids following up with treatment. There are I believe some innovative pilot programs underway for working with the most vulnerable (and sickest) populations that show promise.
Fourth, treatment for asthma has made great strides in the last 30 years or so. I had many sleepless nights as a child taking in effect a stimulant (Tedral) and sitting up against the pillows because if Lay down I couldn’t breathe. In the 80s and 90s with rescue inhalers I still had several ER episodes where they would inject me with epinephrine and put me in a Prednisone taper.
I have not had a single episode since being put on a generic equivalent for Advair, and where rescue inhalers used to last me a couple weeks, now I use them so rarely my last one I had to toss cuz I realized it had expired!
I don’t know what of these meds, cuz Advair is a steroid, they prescribe to children. It would take an intensive investment of time however to reinforce the shift from taking a medication reactively when in need to prophylactically. In a chaotic world with so many urgent unmet needs what tends to be salient is the crisis of TODAY. (And no, not judging, I would do no better.)
As to ADHD, I won’t wade in other than to say that one of the grossest health injustices of our time is to pathologize the NORMAL, self-protective responses of children to the pathological surround they live in. I have worked with many kids who were glibly diagnosed with ADHD (and bipolar disorder) on the basis of behaviors that were clearly symptoms and not the underlying problem. They signalled a need for a change in the toxic environment and support in managing the intolerable feelings it stirred up. Meds in some such cases can be necessary, but they are not sufficient.
Thank you, ChiGal.
As to ADHD,
We’re all on that spectrum, somewhere!
Why do we do the things we do?
Robert Sapolsky has, to my mind, the best current understanding of the genetics of behavior. In a recent book:
Behave: The Biology of Humans at Our Best and Worst
If you have the time, watch lecture series (Stanford course).
Lecture Collection | Human Behavioral Biology [YT]
Stress has very insidious effects, including very Lamarkian ones! See Dutch famine of 1944-45.