One of the many ways in which America is like a third world country is the lack of government support for elder care. And it isn’t as if this is an issue we ought to be ignoring. The number of Americans over 65 will double from 2000 levels by 2040, and the number over 85 is expected to increase fourfold. 70% of the elderly will typically need assistance, which means either going to what is politely referred to as a facility (either a nursing home or “assisted living”) or aging in place with support.
Not surprisingly, most want to remain at home. With Covid turning nursing homes into isolation wards and potential death traps, even more families are trying to find ways to keep elderly relatives out of institutions. But as anyone who has been through this situation knows, this isn’t easy. Most adults aren’t able to dedicate the time, even if it’s something as minor as shopping, some meal prep, escorting them to doctors (and in the old normal, to a hairdresser and for social events), and performing or arranging for house cleaning and maintenance.
And that’s before getting to dealing with older individuals who are feeble and/or cognitively impaired. Care for them often involves bathing, continence issues, lifting them, and dealing with moods swings. Aging is no fun and the elderly can take out their frustrations with their lack of control on those around them.
The responsibility for this care now falls mainly on family members. “America, unlike most developed countries, lacks a comprehensive national long-term-care support or insurance system,” says Bruce Leff, M.D., a professor of medicine at Johns Hopkins University School of Medicine. It’s a hodgepodge of family support and self-pay care at home, plus other private-pay options such as assisted living and short-term skilled home health services. (Nursing homes are mostly funded by Medicaid.) Family members often end up stitching together a patchwork system by hiring private aides, tapping local resources, and providing hands-on help.
And the underlying dynamics aren’t getting better:
But this ad hoc system could be headed for a breakdown with smaller families and fewer children to take on the burden compared with previous generations. In 2010 there were 7.2 family members (potential caregivers) for every person 80 or older, according to a 2013 study by the AARP institute. By 2030 that ratio is expected to drop to 4 to 1.
Needless to say, this situation would seem ideal for companies who provide at-home services for the elderly for those who have the ability to pay. If you watch cable TV, you might encounter ads that are clearly targeting children of aging parents, particularly ones who don’t live nearby.
As I’ll explain, these services look like a lemon market. And the price the intermediaries charge while not being willing or able to assure quality is a big part of the problem.
Lemon Markets
The Market for Lemons, a 1970 paper by “Nobel” Prize winner George Akerlof, is widely recognized as one of the seminal works on information asymmetry, as in why markets don’t operate as well as textbooks say they should due to buyers and sellers having different information.
Akerlof’s example was the market for used cars, where he looked only at buyers and sellers (as in he didn’t put the used car dealer as intermediary into his model). The seller knows how well he has treated and maintained his vehicle, meaning whether it is a lemon or a peach. The buyer has only crude proxies, like the total milage.
Akerlof posited that the buyer, unable to judge the quality of the car, would offer only somewhere between a peach and a lemon price. Owners of peaches would not sell because they would deem the price too low; only lemon owners would. The resulting tendency towards lemons would tend to drive prevailing prices lower, with the result that lemons would dominate the market.
Now in real life, some peach holders would sell at a price they knew to be too cheap because they really need the money. But you get the general point. Markets with lemon tendencies have average prices that are too low for high quality products/services, but those with better goods can’t readily prove that they have better wares.
Home Health Care Agencies as Lemons: Evidence
In the last year, I’ve dealt with three agencies in Birmingham, all of which were supposed well rated (more on those ratings shortly). Despite my lack of any history here, I’ve been forced to hire aides directly, which knock on wood is working well so far.
Note that the “health aide” part of the typical designation is a misnomer. These agencies might have an actual nurse in the adminisphere; we once by happenstance did have a terrific aide for a couple of shifts a month who worked mainly as a nurse in a local hospital. Medicare now provides reviews of what it calls “home health agencies”. But if you click through on the list for Mountain Brook, all provide nursing and other services, like physical and occupational therapy, in addition to “home health aide”. You’ll also see that Medicare rates their costs based on “an episode of care,” reflecting that these firms are mainly in the business of providing relatively short term (say post op care and rehab), higher skilled, higher paid services.
I should add that despite my mother being infirm (she was earlier using a walker and is now wheelchair bound, needed to be bathed, needs help with dressing and “transferring” as in getting in and out of her chair), the demands for her care are not bad: taking her to and from the bathroom, getting her out of bed at the start of the day and helping her with her bedtime prep and getting her into bed, getting her meals (which does not entail any cooking), picking up her mail, cleaning three counters and sinks, loading and unloading a dishwasher, emptying garbage cans, making her bed, doing laundry once a week, and foraging. The worst tasks are her sponge bath and changing her Depends (she does not have incontinence problems but dealing with adult diapers is what it is).
I had been loath to go the route of direct contracting due having no way to find caregiver plus believing that the agencies provided meaningful value added services:
1. Screening and training aides so as to assure a decent quality of care
2. Providing backup if an aide missed a shift (which happens quite a lot: getting sick, car trouble, family crises)
3. Sending bills for reimbursement to my mother’s long-term care insurer (some take assignment of benefits, others bill her but also submit their paperwork to the insurer)
1 and 2 have been a bust. Agency 1, which we hired when we needed only day shifts, could not staff Sundays and had only one aide that was adequate to the task (and that was with her taking awfully long smoking breaks in her car and when running errands, which was still not great given that my mother was ambulatory then and a fall risk). She regularly came when sick and would cough all over my mother, who has COPD. One day my mother blew up and fired the agency over the aide’s unwillingness to skip a shift when unwell despite my mother’s repeated requests.1
Agency 2, a franchisee of a well-known national operator, was a bit better at staffing Sundays. However, after her fall, when my mother needed evening shifts, they had difficulty filling those reliably. On top of that, we got an early warning of their priorities, which was to favor aides over clients when there were difficulties. One aide put over $200 of her clothing charges on my mother’s credit card. When we told the agency, they promptly removed her from us but told us they had concluded it was “an innocent mistake” and assigned her to other clients.2
We had a second case of an aide playing fast and loose with my mother’s card, first putting $50 of her food charges on it and giving us $50, then buying things that she “knew” my mother wanted that she didn’t. The aide got angry at the idea that her judgment was incorrect and even if it had been, she should only be making specifically authorized purchases.3 Despite working as a lab tech during the day, she would also get visibly annoyed when I reminded her to wear her mask over her nose.4
We had also had trouble with about half the new aides sent by this agency not performing basic tasks, like unloading the dishwasher or cleaning the sinks and faucets, which I regard as an essential Covid protection.5 I had to ask for several aides to be replaced because they were unwilling to execute the agency-agreed minimum tasks and gave me ‘tude when tried reminding them.
This agency was also poor about backup. If someone missed their sift, >80% of the time, we were on our own.
Agency 2 effectively fired us, saying only five aides were willing to work with us and limiting us to only those five, which meant we assured of having no backup. And the claim that there were “no more aides” was false, since we learned from the head of Agency 3 that agencies bring new people all the time (my sense from her mention of her recruiting needs is over 10% a month).
Agency 3 was a franchisee of yet another chain. This one hired only aides who were at least Certified Nursing Aides and provided them with more training than Agency 2. They were also better about their backup protocols. Initially things were smooth but started going pear-shaped after a month. They too had difficulty staffing Sundays and regularly scheduled 13 hour shifts, with the result that aides would sometimes fall asleep during their shift.
We had three cases of abandonment. In one, the aide walked off the property (my mother has nearly an acre). I yelled after her since my mother needed to go to the bathroom. She didn’t answer; she was apparently out of earshot. I had to call the agency and have them ring her cell to get her to return. What if I hadn’t been there?
The second case was when an aide they touted as having been with them for years, three times her very first day, left my mother on the toilet in her bathroom. This wasn’t a matter of respecting her privacy and going into the next room. This was during the day, when I normally am sleeping, and I heard her yelling, which would never have been necessary were she close by. The third time, my mother yelled repeatedly. I stuck my head out of my bedroom and yelled at the aide, who said she was in the living room, meaning on the other side of a long narrow house. WTF?
The third time, the aide left my mother alone for 45 minutes. No explanation.
We also had one of their supposed best aides break a chair. Even though the aide flipped the chair over, telling my mother she was cleaning under it (as in trying to fix it), we were told the chair was already broken (false, as our handyman and cleaning service could confirm) and we were made the bad guy. The offer to pay $100 toward a repair or replacement was rescinded.
Agency 3 de facto fired us by asserting word had gotten out, no aides would work for us,6 and they’d need to increase our rates by 50% to fill the shifts. They also tried to put the claim through retroactively and without the notice period stipulated in their own contract, and so I had to remind them of their own contractual obligations.
Home Health Care Agencies as Lemons: Theory
So why is it so hard to hire a good agency? I doubt they exist. And here are some of the reasons:
Large captive audiences and poor oversight
High charges by agencies relative to their value added resulting in poorly paid, very mixed quality aides
High turnover among aides, with better aides likely seeking to work directly for clients
Inability to achieve higher service standards, charge higher rates and pay aides markedly better assures overall mediocrity (at best)
Large captive audiences and poor oversight. The reason I had been loath initially to try to find aides myself, on my own, was having zero local contacts. And it’s not easy even when you do. For instance, a good friend in another state had to organize care for her mother, who had Lewy body dementia. She eventually got two terrific caregivers, one of whom was a live-in, but had to fire three who didn’t work out. I was concerned that I couldn’t find a big enough pool to work through to find who might stick.
Needless to say, my out-of-state friend and I were both close enough to manage the situation. Many older people don’t have relatives who live near enough to keep good tabs on what the agencies were up to. And one big reason I am sure I had so much difficulty is the agencies aren’t used to having monitors. I’m unusual in being in the same house, albeit awake during only one of the two shifts.
Moreover, my mother, like many women of her generation, is terrible about making demands or being critical, until she’s had enough and blows up. And being physically dependent and hard of hearing isn’t conducive to taking on slipshod care. So I suspect that many people in her situation, who’ve hired agencies with their family at a remove, will put up with not great care because they lack the capacity to do anything about it.
High charges by agencies relative to their value added resulting in poorly paid, very mixed quality aides. Agencies take a big cut. We pay $21 an hour an the aides get only $10 an hour. You might now say: “Well, what do you expect for $10 an hour?” but I found out about the appalling net pay only by accident. I had earlier assumed the aides receives something low but not terrible, like $12 or $13 a hour.7
Remember that two of the three agencies we dealt with were franchisees. One in addition to a raft of up front charges, has two fees set as a percent of revenues: a 5% franchise fee and a 2% per month “marketing fee” plus other charges. The other seems to do less nickel and diming and as best as I can tell, has a “royalty fee” and “marketing fee” that total 8% of revenues. That’s a pretty healthy skim off the top.
The agencies do little to some training. Agency 3, which has a CNA as a minimum requirement, said Agency 2 gives only a day of training; they provide several days.
So where does the $11 an hour go, aside to franchise fees and overheads like rent and accounting, 24 hour phone coverage, and scheduling? It seems a big cost is recruiting all the time. The head of Agency 3, which has about 140 aides, was screening 10-15 people every two weeks. She didn’t tell me her target for net hires.
You might reasonably say, why don’t the agencies charge more so they can pay better, reduce turnover, and differentiate their brand locally? Agency 1 was charging more but their staff was no better than the other two agencies, and for all I know, the price differential was going straight into the owners’ pockets. Agency 3 is trying to hire better (or at least more credentialed) aides and train them better, yet they are not commanding a price premium.
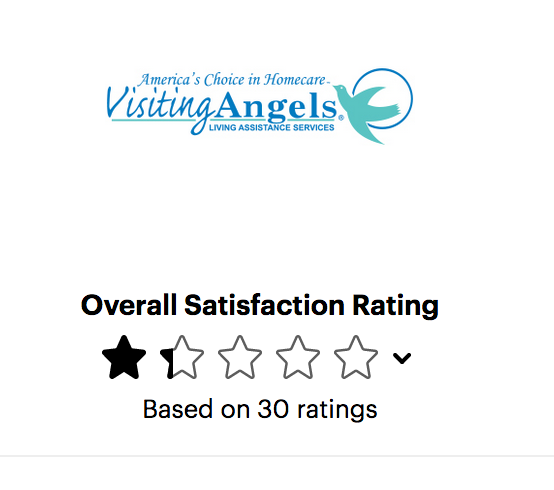
One constraint is the lemon problem: customers like me can’t tell from the outside what the service quality is like. National ratings are across a huge number of franchisees and tell you nothing about your local operator, but they do warn you these services generally suck:8

Local ratings are not much more help. Here, they are much higher, but they also cluster between 4.4 and 4.7 out of 5. Worse, they look manipulated. Many are openly from employees, about what a great place XYZ is to work, making one wonder how many of the rest are from employees pressed to pump the score and who did so more artfully.
But another problem with raising prices is what the market will bear. We are a bit price insensitive since my mother has a good long-term care policy with a pretty high total policy limit. However, her policy also has a total daily maximum which is too low even to pay for the full day rate for nursing home care in Alabama, where your health care dollar goes a lot further than in most of the US. It’s also way below the cost of 24 hour care at home, which her doctor has long insisted on. Look at how the costs rack up even if you are talking just 6 hour daily shifts. From Consumer Reports:
In 2017 the national median cost for 44 hours a week of nonmedical home-care services was $47,934 per year, according to Genworth, a long-term-care insurer.
Pull out a calculator. The average cost in 2017 was $20.54. Admittedly Genworth will pay for both agencies and independent aides, but these national costs were also incurred all over the US, where wage rates are generally higher than here.
High turnover among aides, with better aides likely seeking to work directly for clients. As indicated, there’s a lot of churn. Some of it is due to the aides in many cases having their aide duty as a second job (a couple of the best aides we had worked only 2 shifts a month and we happened to get them). So if they get more hours at their main gig, they’ll abandon the aide work. Some are using the aide shifts to work more than 40 hours a week to save money for a special purpose.
But the “better” aides who might want or need to keep at this sort of thing regularly presumably work out that they are a cut above the norm and find a way to be hired privately. The difference between $10 and $21 an hour creates a lot of price points for a “win/win” situation. The agencies try to impede worker-poaching via draconian language in their agreements with clients (and the head of Agency 3 also said in their agreements with aides) to prevent aides from going to clients.
Like our our out-of-state friend, most people who could would do better to go the direct route. But I have to stress that for anyone with parents more than a couple of hour drive away, it would be very difficult to set up and manage independent caregivers.
In fairness, one of the things that makes it hard for agencies to get ahead in this game is that even a CNA certificate isn’t a great predictor of what makes for a good aide. As you can see from the shaggy dog stories above, we had ones from Agency 3 that were train wrecks.
The most important considerations are a good work ethic, common sense and a reasonable level of intelligence, some training like how to lift someone (which an otherwise unskilled person can learn from an occupational therapist), and a pretty even keel temperament. It’s hard to screen for that in a recruitment process. Even fancy firm employers have been forced to admit their hiring processes aren’t good at sorting candidates well, despite all the energy they devote.
____
1 Agency 1’s management had ‘tude and also charged more than other agencies. They managed to extract a further premium for the one aide that was not bad, despite her not having any credentials or even a high school degree. Our insurer Genworth somehow organized for them to start with us and my mother suspected that there was a kickback to the employees involved.
2 This was clearly bunk. I happened to be in the room when my mother found the bogus charge on the card. The aide, who was sitting next to my mother, didn’t even look at statement to see the date or amount but immediately confessed. She clearly either made the fraudulent charge knowingly or realized immediately afterwards that she’d made a mistake. But rather than tell me or my mother so we could straighten things out, she had decided to see if anyone would catch her out. In other words, if this was a mistake, it was not innocent.
3 I am sure Clive will go nuts over the idea of letting a third party put charges on a credit card, but this practice is pervasive with the housebound elderly.
4 I also had trouble before masks were mandatory at businesses getting aides from this agency to wear masks, even though we provided them. The agency would not support my efforts to get compliance.
5 Before you try, “Why didn’t you unload the dishwasher?” the agency has a list of duties they agreed the aides were to perform and this was one of them. And I am not going to stoop to give other reasons. I have reason to believe that the second aide who misused my mother’s credit card decided to get in front of the issue before I could Say Something and complained to the agency about my rather long conversation with her trying to get it through her head why she couldn’t make charges willy-nilly on my mother’s card. I did not raise my voice, but New York directness is regularly seen as aggression down here, particularly from women.
6 We had some aides who worked regular shifts who got on fine with us, so this claim was at best considerably exaggerated. However, my yelling across the house at the aide who left my mother in the bathroom was twisted into a charge that I yelled at aides, which was narrowly correct but clearly misleading in context (there was another instance where I yelled across the house because a different aide from this agency wasn’t answering the door for a repairman visit I had told her about in writing; the aides get notes from me every AM before I turn in. And they should be answering the door whether I leave a note or not).
7 A living wage here is $11.88 an hour for a single person, $9.24 for a couple with no kids and both working, and $12.81 for two working parents with one child.
8 We used the local outfit for one of these two franchisors.


The UK has very little provision as well. Its very difficult. The problem is far worse when you love and respect the elderly person. Because the system embeds humiliation and horror at so many stages. Watching your parent suffer unnecessarily because there is little care or infrastructure for their care terrifies me.
I hope I have the money to afford a Japanese designed toilet for the elderly if I am unlucky enough to live that long.
Why a Japanese designed toilet?
There are great toilets all over Japan in hotels and other places tourists go. They have warmed washlet seats and are well designed. We bought Toto brand for our house. Don’t know specifically about for the infirm.
Thanks. I have seen just the seat available for a few hundred dollars at Costco occasionally. I assume it means you wouldn’t have to wipe for the elder after use?
I think this is precisely why in some many countries (mostly Middle East and Asia) families who can afford it hire full time live in care assistants from poorer regions/countries. This can of course be a very abusive system in all sorts of ways (sometimes close to slavery), but it gives the families control over who is looking after their elderly relatives.
Here in Ireland, the government had what in many ways was an admirable scheme of hiring older women who were out of the job market for a long time and training them as home assistants. It was intended to give a double benefit, of helping poorer women with little skills find meaningful work, while providing a better range of home visits for the elderly. But my mother found the negative side of it – she was allocated a home care assistant who would visit three times a week, supposedly to check in, do cleaning and cooking, and so on. My mothers observation on it was ‘I thought she was supposed to help me, not to other way around’. The assistant had come from an abusive family background and loved to visit my mother – her visits involved her making a pot of tea and sitting down for 2 hours to tell my mother all about her problems.
As to the broader problem of the ‘lemon market’ in home care, the only solution of course outside of direct government provision is strong independent regulation. But this is very difficult, and adds a lot of cost and bureaucracy to the system. And regulation in healthcare has an unfortunate history of being manipulated for the providers benefit (by, for example, eliminating less well resourced competition). There are no easy answers.
This is the same here in Germany. Women from eastern Europe. There are agencies which find and place them, but after placement afaik they don’t get a recurring fee.
Has been going on since the 90s and the women come from farther east now, e.g earlier times it was Poland, Romania. Turnover is still high however.
As for the US: wouldn’t that be a typical employment for an illegal from south of the border?
Don’t know about the whole market, but I do know that CZ, Slovakia and Poland suffer from lack of nursing staff, as many nurses decide to do aged care in Germany as just about everything is better, and if you live near the border, it’s just sooo much better.
With those, at least you have real qualified nurses doing it.
As a aside, a lot of them were caught in lockdowns earlier this year, and it was no fun for them…
A high proportion of nurses/nurse aides/assistants here are from the Philippines or Karala in southern India. Many have children and family at home and it may to 2 years or more before they can travel back for a visit. The personal stress for many of them must be terrible.
Can’t they import care staff from further east: Ukraine, Belarus and Kazakhstan? Or maybe Syria or Libya where NATO has created an excess labor pool that is up for low bid? Its a free-for-all market, isn’t it?
No. Poland and Romania are EU members, so at least since 10-15 years ago, all have the right of free movement and employment in other EU countries. Farther east it’s outside the EU and therefore it’s much harder or you would have to work illegally or as an asylum seeker which isn’t allowed, at first, to work..
Ukraine, Libya, Syria would work fairly easily, Belarus, Kazakhstan no: no official war there. Also the Syrians, etc. wouldn’t work in that field: not too many women, less of them come for actual work purposes. And the prospective employers probably wouldn’t like them either if they did.
With the number of elderly people on the increase I would say that it is only a matter of time until nearly all the home health care aide companies will be brought up by private equity companies who will then squeeze every dollar that they can out of every client as it will be so profitable. I have no idea what elderly people do that have to make these decisions by themselves without loyal children intervening to take the stress out of these situations.
Come to think of it, here is another horrible prediction. When private equity companies have brought up most of these companies, they will then seek to use prisoners on day-release programs hired from the States as home aides as they will be cheap to hire and will have incentive to behave themselves with their clients. Tell me that this will never come to pass.
It will not happen for two reasons:
Making people who are in prison due to mainly poor impulse control work with eldery people who are very hard to work with: dementia makes them cranky, stubborn and often very abusive is a recipe fr disaster.
Second, there are enough jobs which are unwanted, dangerous, poorly paid, etc. a prisoner could do. No need to make them work in ones that need lots of empathy and where you can import people working for low wages from overseas. Importing people to do these kinds of social jobs is much easier than to convince an employer to let a violent con support grandma.
The amount of hassle for possibly resulting murders, beatings, etc. of old people are not worth it and more importantly are too expensive.
One thing that’s included in the differential between their pay and what you’re charged is the statutory benefits (Social Security, Medicare, unemployment insurance, worker’s compensation). FICA is 7.65%, Alabama’s SUI rate is 2.7% for the first $8,000 paid, FUTA is 6% for the first $7,000, and a quick search suggests a cost of 2.75% for worker’s comp in Alabama. That adds up to 19.1% (given the high turnover, I’m reluctant to assume you’ll only pay $216 and $420 for federal and state unemployment).
Despite the training, I have the sense that some of these agencies are playing fast and loose. The two agencies each “employ” enough people that they ought to provide health insurance but I know for a fact that none of them do. They could be working very hard to keep them below 30 hours a week/130 hours a month.
If you are not part of the solution, there’s good money to be made in prolonging the problem.
Wow, I was lucky.
When I was looking I was told local churches where a possible place to find someone directly and did sort of have luck there. I did find a woman but she was snapped up by someone else just before I contacted her. And the next person I found via a church had cared for someone for several years who had very recently died and decided that she needed a break from the emotional turmoil.
In the end I used Home Instead and had no problems. As you state it must really depend on the local franchise. But it was daytime care only and my Mom only needed assistance in dressing/bathing. I had one lady who came for several years with an occasional backup that was usually someone new.
After a few years my Mom had to go into a memory unit, which I was again lucky as I found one about 100 yards off the route I could travel to and from work. I dropped in pretty regularly for a few minutes in the morning or evening and, upon occasion I would see the person who used to do the daytime care in the visitor logs.
I think Yves is right to characterize it as a market for lemons. In my experience, the only way to go is to find a live in carer and to keep tabs on how the parent is doing. We tried agencies but they could not solve our problems. The staff always have an incentive to “double dip” – work as many elderly as possible and short change the cared for in terms of hours worked. The good ones did this as well as the bad ones.
And thats abstracting from the really bad ones, who were rejected for rudeness, or incompetence or simply not wearing PPE.
There is a prize coming for the business that finds a way to solve this problem.
My wife has had home health aides several times after stays in the hospital or rehab nursing homes. Our experience was both good and bad. The best help was from our county department of health. Private providers have been mostly not that great or dependable. You are right about quality. We got both good and bad help from the same private agency.
Caregivers subsisting on minimum wage (or less, due to agency shenanigans and looting) have little incentive in the dog-eat-dog US to “excel” in their work. Low-status, low-pay, and demanding management, with little to no regulatory oversight, is not a recipe for quality care. And from experience my wife had as a home health aide and CNA and then home nurse for special-needs children, the “families” are often demanding and abusive and expect not just peaches but pearls for the lemon prices they are willing or able to pay. She was conscientious to a fault, often came home exhausted and in tears from the double whammy of nasty family members and Simon Legree managers. Fortunately, she was able to move into work as a clinical nurse (with another set of horror stories, of course.)
I see a PE market for ‘assisted suicide parlors,” where old farts driven to despair by conditions where there is no “quality of life” can check out. PE has already gone into the hospice racket. Lots of looting opportunities in this best of all possible exceptional countries, https://hospicenews.com/2020/06/24/covid-is-delaying-private-equity-hospice-transactions/
Holy smokes, thats right next to the poverty line where I live. I’ve visited Pell City/Anniston and noted the working poverty. Its no great surprise that manufacturers/suppliers for the auto industry would choose to locate their plants in the low labor cost area (a la Jack Welch) to maximize their gains.
This link doesn’t address home health aid problems directly. It’s a good starting place for local eldercare resources. Type your zip code into the search bar and the list of Medicare approved sources for your area are displayed. Might be a useful starting point for some questions.
https://eldercare.acl.gov/Public/Index.aspx
As indicated, I displayed the link for my ZIP in the post, and the agencies are all primarily in the business of providing private duty nurses and other specialists, like occupational and speech therapists.
Oh hi! I used to work as a licensed nurse assistant and private caregiver. I really enjoyed the work but there were several things which made it untenable as a long term career. It’s virtually impossible to get time off (even unpaid). If you are working day shift M-F there are occasions when you need time off, like medical appointments, trips to the DMV, and maybe even a leisure activity. Its incredibly discouraging to ask for time off in advance and be denied because there is no one to cover for you. Working at a hospital the expectation was that we would work three 12 hour shifts per week, a mix of days and nights and every other weekend. These expectations and not being provided with any sort of set schedule made it virtually impossible to obtain childcare. Reliable, smart workers see these two things and leave for greener pastures. I got a BS degree and a salaried job. If I was treated half as well at the caregiving jobs as I am at my IT job I wouldn’t have left.
I believe the Government paperwork as much as the cash outflows for taxes serve as a barrier to new providers — especially individuals — entering the market to provide home health services. Many states add licensing and bonding requirements that bump up costs for small scale providers — Florida required services providing temporary nurses to hospitals to have a licensed nutritionist on staff. Even given these barriers providing in-home nursing services would seem a natural as a workers-coop business.
I suspect the companies providing home-aides are not too different from the companies providing contract engineers. I remember engineers set up small contracting firms to exploit any contacts they established. In response contracting firms compelled their contractors sign non-compete agreements to stop that practice. If a contracting company plays fast and loose, a not uncommon practice of the contract engineering firms, the IRS had a nasty way of coming after their money from the company who purchased the contract services which I suspect the IRS did this especially when a 1099 or a small contracting house was the culprit. This shutdown a lot of 1099 activity — contractors working as their own contracting service — and was one of the reasons the big companies started dealing only with large contracting houses and shut out the little guys.
I’m dealing with similar issues with my 93-year-old mother who recently was diagnosed with congestive heart failure. After her meds and dietary regimen were changed by a caridologist she has improved markedly but still needs help in the daytime. We feel very lucky to be in a small town where people know my mother and we have some wonderful caregivers who are competent, trustworthy and nice people. We have not had to deal with an agency.
My mother pays them $20 an hour under the table which really adds up, but at this point it is still cheaper than most care homes and with that kind of pay we have several competent people to choose from. Luckily mom can afford this thanks to my late father, who was thrifty and left her in good shape financially. Yves you might not have time for this, but asking around in the local community about trustworthy caregivers and then dealing with them directly might pay off.
I had good luck finding help by asking people who work in elder care facilities if they knew any co-workers who wanted to take a private job. The ones who do form an informal network and can find their own substitute coverage for time off.
Our mom is 93 and now in a small 5 resident assisted living home that seems well run.
Trying to manage home care was very difficult. 2 siblings live nearby, 2 long distances away. Mom resented helpers being present and would run them off. Some we OK, others somewhat lazy. All were individuals, no agency. Pay was $12/hour in New Orleans. Mom had the notion that helpers should have been doing heavy house cleaning and outside chores (cleaning rain gutters???).
What put an end to the stay at home was 8 hours simply wasn’t enough and we couldn’t figure how to cover the obvious need for 16 or 24 hours. We also had occasional coverage problems. The helper might help her bathe, then mom would bathe again, alone, in the evening. There were considerable mobility and memory problems. Medication was often missed and she was eating very poorly. The AL place has managed all these things well ($6000/month).
Families are REALLY on their own providing elder or disabled care. What haunts me is I’m 66 and we have a disabled son. Even if you have financial resources, the logistics of care provision are difficult. How we manage our own care and our son’s in coming years keeps me awake…
6000 per month
Wow, just wow.
For full-blown alzheimer’s, fees run $100-120K per year at a decent nursing home. The for profit medicaid nursing homes double up residents, pay near minimum wage and have terrible quality of care and bill NYS almost as much.
My partner’s father has moderate stage Alzheimers. It is on the verge of progressing into late. They are trying to keep him at home as long as possible due to high cost and notoriously poor quality care. My partner has put his/our life on hold for 6 years now to live with his parents to take care of his father in order to keep him out of a nursing home. He hasn’t worked a traditional job since moving in with them-he has been a full time carer for his father. Recently it’s been getting to be a lot and he’s finally been voicing his frustration and tiredness to me. He’s getting run down, esp since covid put the kibash on the short 1-2 hour programs for patients that would happen once or twice a week. I don’t know what the next 6 months will bring.
Sorry to hear about your (all too common) conundrum Yves. If you lived in NYC, Washington state, or rural Wisconsin I’d have some suggestions for you, as those places have worker co-op home health agencies (Cooperative Home Care Associates in NYC is actually the largest worker co-op in the country). We need a lot more of them, but unfortunately, they are difficult and expensive to set up. CHCA, Capital Homecare Cooperative (WA), and Cooperative Care (WI) are the only three I’m aware of in the US.
Family story: My sister in law went through 5 or 6 agency hires, none of them were good workers or even reliable until one, a girl from Ethiopia, applied. She was a great worker, and very skilled so they offered her a live-in position which worked out for almost a year. She left for family reasons. After that they hired an old school friend also as a live-in; she had nurses aide skills and was very reliable. She stayed with them for several years but she occasionally brought her grandchildren over when she couldn’t find anyone to watch them. Hiring her privately worked for everyone. I’d think hiring a good live-in is the best way to go. They get the extra benefit of room and board plus a paycheck. You get better peace of mind.
I went through this for years! My mother was so nasty to aides, they seldom stayed long. Sometimes, you can ask nurses at the hospital or nursing homes if they know someone willing to moonlight. I had to have separate people to clean, and none would even microwave a prepared meal. When I last worked in home care,, I made $8 an hour while they charged patients $25. Also, made them sign a contract for 3 months, up front, a big hardship for many.
This brings up memories of what happened with my mom. She had always been very independent and didn’t like “help” around. Her fall happened when she was 99, and I soon realized that she would need constant care, because she became bedridden. I hired 24-hr home health aides from an agency (I had no idea what different agencies were out there), so it was like a random pick. There was only one really good aide (she worked as a nurse in a hospital), and the others just put their time in. I was at my mother’s home as much as I could be during the day, but I had to go home and sleep. Also, I had the aides keep a daily diary of what they did, and how my mother’s care went. I really didn’t trust them enough to not be there.
Yes, it’s expensive – for two months of 24 hr. care it cost $40,000 (this was in San Francisco). Another problem I had was language issues with the aides. 95% of them spoke English as a second language, so it was hard for me to communicate with them. Home health care is very difficult work and aides should be paid more than minimum wage, and they need more than 2-week training.
I think having a live-in caregiver is preferable – finding someone to trust is also difficult. The U.S. needs comprehensive elder care – such as child care. .
It’s understandable given the intimate nature of the work, but it’s surpising to see Yves cherry-pick data. Yes, agencies don’t add value, but neither agencies nor, in this case, Yves.are willing to pay the people who take care of loved ones anything remotely close to what it takes to live a decent life in this country.
Start here: “A living wage here is $11.88 an hour for a single person, $9.24 for a couple with no kids and both working, and $12.81 for two working parents with one child.”
Ok, NC readers, re-read that sentence. 1) Single person. 2) Couple no kids, both working. 3) Couple, both working, one child, What’s wrong with that selection of examples? Well, let’s add a kid or subtract an income and watch the math change radically.
Not sure where the $11.88 “living wage” comes from, but that doesn’t really matter. The best measure of livability is the Self-Sufficiency Standard (SSS). For Jefferson County Alabama in 2020, it takes $12.34 an hour for self-sufficiency for a single person. For Yves’ two other categories, it’s $9.34 (Couple, both working) and $10.22 – $12.84 (Couple, both working, one child, depending on the age of the child). More or less the ballpark Yves describes.
But that doesn’t really describe the universe of the families of American workers, now does it? So start adding and subtracting. The really useful thing about the SSS is that it shows the different costs associated with families in different stages of life:
One Adult, one child: $15.85 – $21.42 [$15.85 teenager; – $19.36 school-ager; $21.42 pre-schooler; $21.45 infant]. So $12-$13/hour? definitely not ok.
Two Adults, Two Children: $10.19 – $15.65 (there are ten permutations, so not going to write them all down.
One Adult, Two children: $15.89 for two teenagers; $19.35 for one teenager + one school-ager; all 8 other combinations of two children: $22.13 – $27.22
Two Adults, three children: 20 different combinations: $12.05 (all three teenagers) – $19.82, including 6 >$18.00/hr.
One Adult, three children: 3 teenagers = $19.92, all other combos $23.67 – $35.84
and so on. Personally, I’ve always felt that the SSS underestimated health care and other costs, but since it was developed by the Center for Women’s Welfare at the University of Washington in 2002, it’s been the best measure of what it takes to live in the U.S. And remember, often workers in health care jobs have older relatives that they themselves have to care for.
The point is that these personal anecdotes, while valuable in exposing the systemic uselessness of agencies, dramatically discount the economic reality of the people we expect to do some extremely difficult work. LIfting and turning is a recipe for ergonomic injury, especially without training (which in turn, creates elevated risk of opiate addiction, and then banishment from health care professions). The emotional comfort and support that must go with the various tasks is, as family members know, itself grueling.
The failures of the workers hired to care for Yves’ mom shouldn’t be dismissed. But you also can’t handwave “family crises” that make it hard for workers to show up. A single parent with two kids can no more afford reliable child care on $11, $12 or $13 an hour than most of us can afford reliable home care for elderly loved ones. “Family crises” are often things like “my mother fell and had to go to the hospital so there’s nobody to take care of my kids (never mind take care of my mother when she gets out of the hospital).”
The U.S. spends twice as much per capita on average on “health care” compared to other wealthy countries. We go to the doctor and the hospital less often on average than peer countries. We spend incredible sums on nursing home care. The money is there for acute care, rehabilitative care, palliative care and assistive care. All of it. All at truly decent wages. We just refuse to seize the money and spend it collectively on actual health care and family support.
We live in a low-wage trap economy. These jobs — which should especially support workers in stable lives so that they can build relationships with clients — are shitty jobs that create precarious lives, definitely at $12 or $13 an hour and even at $17 or $18 an hour. The agencies are rent-extractors for what should be public services and definitely should go. But there’s a whole lot more.
This is another industry that seems, at least for me, impossible to negotiate. I have gone where Yves has tread, but for myself, not a parent. Things weren’t nearly as dire for me as they were for my now deceased parents, or Yves’s care of her mother. (Although my father’s non-dementia skilled nursing care in northern CA was over 50k per year 20 years ago.)
There were times when, living alone (pre Covid), I needed assistance not provided by home health. What I found was that franchises would give me names, with all manner of disclaiming language, informing me that I would need to undertake my own background checks. I gave it a try, but things became fairly chaotic and I gave up.
Speaking of innocent mistakes and so forth, I was advised by more than one friend to just accept the fact that if I hired home help, things would begin to “disappear.” Yes, it’s a problem.