By Lambert Strether of Corrente
Science is popping! Nature’s editors[1] and reviewers must have had quite at time doing all these papers more or less at once. And it’s certainly encouraging to see Long Covid[2] getting major play. In this simple post, I’ll present the most salient features of each of the four studies (and I’m not super-strong on methodological issues, so I hope readers will bear with me, and mavens will weigh in). Then I’ll look into where the salvo landed.
Presenting the studies in order by date:
1) “The immunology of long COVID“ Nature July 11, 2023
From the Abstract:
Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe. Estimated numbers vary but the assumption is that, of all those who had COVID-19 globally, at least 10% have long COVID. The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new health-care challenge…. There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein–Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation. Thus, the current picture is one of convergence towards a map of an immunopathogenic aetiology of long COVID, though as yet with insufficient data for a mechanistic synthesis or to fully inform therapeutic pathways.
On Long COVID symptoms:
The lists of long COVID symptoms were initially derived through reports from patient groups, leading to a keynote online survey conducted at the end of 2020 from nearly 4,000 individuals across 56 countries that supplied symptom data… [L]ong COVID is a truly multi-organ, multisystem disease, with symptoms that appear to indicate a pathological process beyond and distinct from just the ACE2-positive tissues targeted for viral ingress during the acute infection…. For a disease process with such a diverse array of symptom combinations, the challenge has been whether and how to stratify patients into specific clusters20. Proponents of the approach would argue that this is a prerequisite for the tailored management of such a heterogeneous disease entity; the opposing view would be that such clusters impose an artificial structure on a highly fluid process whereby an individual may be prioritized for referral for neurocognitive symptoms yet may, at other times, suffer considerably from, for example, breathlessness. … n summary, as the field moves towards consensus stratifications that may be valuable for clinical referral pathways, the pressing challenge is to navigate, via specific biomarker testing[3], the relation of clusters to differential mechanisms and pathologies.
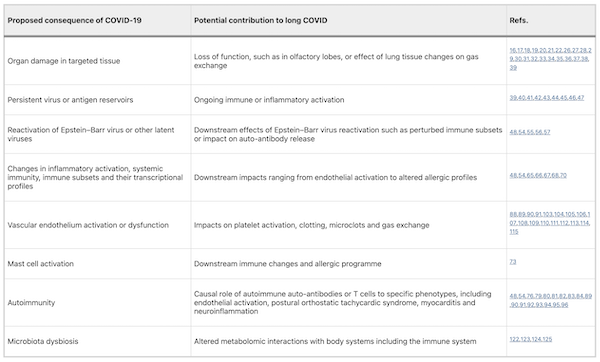
On possible mechanisms: Here is a handy table:
Disease risks:
The clinical definition of long COVID is still a work in progress. Already there is a tendency to draw a distinction between the familiar spectrum of persistent symptoms such as fatigue, breathlessness and neurocognitive impairment, on the one hand, and increased risk of overt ‘lifetime’ impacts such as increased risk of stroke, myocardial infarction, and types 1 and 2 diabetes, on the other. In the absence of clear mechanistic pathways, we argue that both sets of outcomes need to be considered within the framework of long COVID. If long COVID encompasses consequences of the infection beyond 4 weeks, then increased lifetime risk of neurological, cardiovascular, renal or metabolic disease events certainly qualify within the term ‘long’.
Therapeutics and outlook:
It should be clear from the above that, in the few years that it has taken to recognize and define long COVID, a huge amount of high-quality research has been conducted and many aspects of the puzzle of pathogenesis have been put in place. However, it is invidious at this stage to attempt any mechanistic synthesis that could draw the connecting lines between those parts of the picture that seem to be largely agreed… It is apparent that it is premature and spurious to contort these into a simple pathway while such huge knowledge gaps remain. Meanwhile, people with long COVID feel neglected and are impatient to see these medical research findings translated into therapeutic trials…. There is a powerful case for large, comparative, randomized control trials with the transformative potential that the Recovery trial offered for acute COVID-19.
And:
The oncoming burden of long COVID faced by patients, health-care providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it[4]. If 10% of acute infections lead to persistent symptoms, it could be predicted that ~400 million individuals globally are in need of support for long COVID. The biggest unknowns remain the joined-up scheme of its pathogenesis and thus the best candidate therapeutics to be trialled in randomized controlled trials, along with a better understanding of the kinetics of recovery and the factors influencing this. Some countries have invested in first-round funding for the pilot investigations. From the above, far more will be needed.
2) “Long COVID prevalence and impact on quality of life 2 years after acute COVID-19“ Nature (July 11, 2023). N = 132. South Korea.
From the Abstract:
There has been an increasing interest in the long-term impact of long COVID. However, only a few studies have investigated the clinical manifestations of long COVID after 24 months of acute infection…. After excluding the cases of COVID-19 reinfection, 132 individuals were included in the final analysis. Among the 132 participants, 94 (71.2%) experienced symptoms of long COVID. The most frequently reported symptoms were fatigue (34.8%), amnesia (30.3%), concentration difficulties (24.2%), insomnia (20.5%), and depression (19.7%). Notably, no significant differences were noted in the incidence of long COVID at 24 months in terms of the number of vaccinations received. Although the neuropsychiatric quality of life improved over time, it continued to affect 32.7% of participants.
Results. Handy chart:
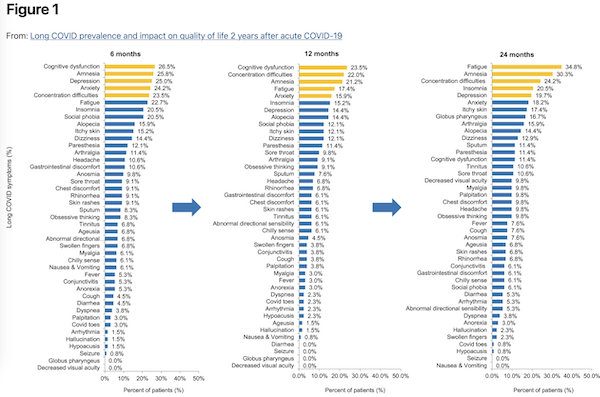
Discussion:
To the best of our knowledge, this is the first study to assess the long-term impact of COVID-19 at 24 months after acute COVID-19 in patients with documented COVID-19 vaccination and without history of reinfection. Based on the findings of this study, long COVID symptoms improved over time and neuropsychiatric symptoms tended to persist longer than other symptoms up to 24 months after COVID-19.
Conclusions:
Although long COVID usually improves over time, neuropsychiatric symptoms can persist for up to 24 months after an acute infection and occur more frequently than other symptoms. Patients with mild COVID-19 disease, who account for the majority of patients with COVID-19, may continue to have a poor quality of life. In addition, the occurrence of long COVID does not appear to be significantly affected by COVID-19 vaccination or the number of vaccinations received.
3) “Gene linked to long COVID found in analysis of thousands of patients“ Nature (July 11, 2013).
The first genome-wide hunt to find genetic risk factors for long COVID has yielded a hit: a DNA sequence near a gene called FOXP4, which is active in the lungs and in some immune cells… The study, which was released as a preprint on 1 July1, used data collected from 6,450 people with long COVID across 16 countries.
And:
For more than three years, the global COVID-19 Host Genetics Initiative has been searching for DNA sequences that are associated with a risk of developing severe COVID-19. That hunt, which is ongoing, has implicated genes involved in the immune system and in allowing the virus SARS-CoV-2 to enter cells.
The long-COVID study is a spin-off from that effort, says Hugo Zeberg, a geneticist at the Karolinska Institute in Stockholm and a lead author of the preprint. To study the condition, the team compiled data from 24 studies involving a total of nearly 6,500 people diagnosed with long COVID, as well as more than one million other participants who served as controls.
In one analysis that combined data from 11 of those studies, researchers found a particular region of the genome that was associated with about 1.6-fold higher odds of developing long COVID. That segment of DNA is near a gene called FOXP4, which is active in the lungs and other organs. The variant linked to long COVID is also associated with higher expression of FOXP4 in lung cells.
Previous research has linked the same gene to an increased risk of severe COVID-19, and Zeberg and his colleagues found that it is also associated with lung cancer. Although having severe COVID-19 increases the risk of developing long COVID, the team found that the contribution of the DNA variant to long-COVID risk was too large to be explained by its link to severe COVID-19 alone. “This variant has a much stronger impact on long COVID than its impact on severity,” says Zeberg.
But:
Replicating that finding in other data sets would help to strengthen the study’s conclusions, says Zhongshan Cheng, a bioinformatician at St. Jude Children’s Research Hospital in Memphis, Tennessee. Many of the data used in the long-COVID analysis were also used in the analysis that found a link between FOX4P and severe COVID-19, he notes. Fresh data would help to rule out the possibility that other factors, such as lung cancer, could have influenced the apparent association with FOX4P.
4) “Natural history of long-COVID in a nationwide, population cohort study“ Nature (July 13, 2023). N = 160,781.
From the Abstract:
Previous studies on the natural history of long-COVID have been few and selective. Without comparison groups, disease progression cannot be differentiated from symptoms originating from other causes. The Long-COVID in Scotland Study (Long-CISS) is a Scotland-wide, general population cohort of adults who had laboratory-confirmed SARS-CoV-2 infection matched to PCR-negative adults.
Introduction:
Understanding the scale and natural history of long-COVID is essential to planning health and social care. The majority of studies report the prevalence of long-COVID at a single timepoint post-infection, with some adjusting for pre-existing symptoms. Less is known about changes in long-COVID over time…. [W]hile long-COVID may be a stable condition in some, existing evidence suggests that others may experience recovery, relapse, or progression. We use serial questionnaire data from the long-COVID in Scotland Study (Long-CISS)20 to investigate the natural history of long-COVID in an unselected, general population cohort with laboratory-confirmed SARS-CoV-2 infection compared with symptoms in an age-, sex-, and socioeconomically-matched group of people who have never been infected.
Recovery Status: Handy Table:
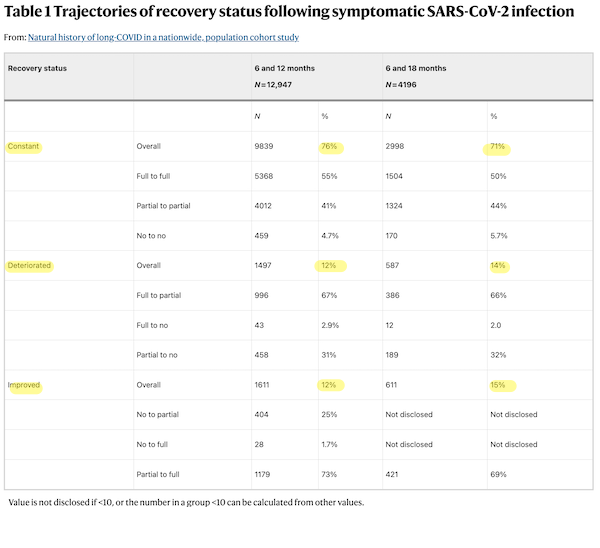
That “constant” seems pretty grim.
Discussion:
This study reports the trajectory of long-COVID in the general population compared to contemporaneous changes in symptoms and quality of life in a comparison group that had never been infected. Beyond 6 months following SARS-CoV-2 infection, there was no significant overall change in either self-reported recovery status or the percentage of people reporting at least one symptom known to be associated with previous SARS-CoV-2 infection. However, 12% of people reported improvements in their recovery status, and 12% reported deterioration. These different trajectories were driven by different symptoms. In some people, altered taste, smell and confusion (‘brain fog’) resolved over time whereas others reported late onset dry or productive cough and hearing problems. These changes were not explained by underlying trends or confounding. Our findings demonstrate the importance of exploring individual symptoms rather than only grouping them together as a composite outcome.
And on class:
Socioeconomic deprivation and depression are known to be associated with development of long-COVID. Our findings elaborate by showing both to also be associated with reduced risk of improvement over time and increased risk of deterioration. Biological mechanisms may partly explain these observations. The relationship between depression and inflammation is bidirectional. Novel immune therapeutic targets are being investigated for the treatment of depression, and there is a well-documented link between acute or chronic psychological stress and immune markers. The stress resulting from socioeconomic deprivation has been linked to changes in immune response and wider detrimental health effects. However, in this study, socioeconomic differences in self-reported recovery status were not corroborated by different changes in specific symptoms over time, other than a weak association with hearing problems. Therefore, it is also plausible that more deprived groups have less capacity to adapt their lives to ongoing health problems or poorer access to support.
Conclusion
One would think that Nature’s salvo would, well, land somewhere. Let’s check out the coverage. This is July 13; the “The immunology of long COVID” was published on July 11, more than enough time to the mainstream press to pick it up, if not the New York Times, the Wall Street Journal, or the Washington Post, then MedPage, or Becker’s Hospital Review, or generalist publications like Salon, or New York Magazine. One would think. This is a great quote, well-adapted for virality:
The oncoming burden of long COVID faced by patients, health-care providers, governments and economies is so large as to be unfathomable.
That’s the sort of quote that should appear in an article! Let’s search on “so large as to be unfathomable” over the last week:
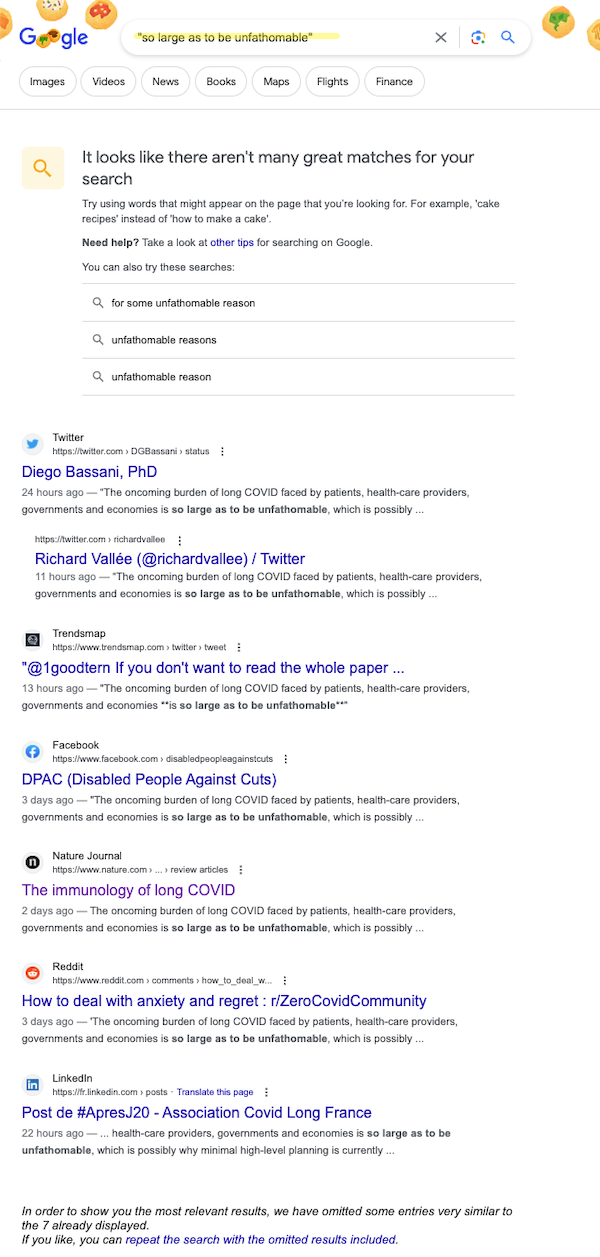
Seven (count ’em, 7) hits: 3 from Twitter (thanks, Elon!), 1 from Facebook, LinkedIn, and Reddit, and 1 to Nature’s paper itself. Perhaps we’ll have better luck if we search on the title. Perhaps:
And page 2, of the two pages of hits:
Once again, mostly social media, a smattering of other sites, and no coverage at all from the majors, or even the minors (or the minis).
Two days is more than enough time to react to a major paper on Long Covid; journalists transform scientific papers into stories all the time. We’ll have to see what happens in the next few days, but if nothing does, it will be hard to conclude that there’s no censorship going on.
NOTES
[1] Altruism is not one of the most salient features of the scientific publishing industry. So I want to give a rare shoutout to the majors like Nature, Science, JAMA, NEJM, etc., for dropping the paywalls on so many Covid articles. This was truly public-spirited act, and many people, including me, learned a tremendous amount, not just about Covid, but about reading the literature. Of course, a reversion to the mean is on its way, but it was good while it lasted!
[2] It’s interesting that Nature’s editors decided to use “Long Covid,” instead of “PASC (post-acute sequelae SARS-CoV-2 infection)” as in the ridiculous and bad NIH squillion-dollar “12 symptoms” paper. (I’m omitting a Swedish paper from this same week on “post Covid” in young adults, because the symptoms are different, and the time period is shorter.
[3] Defining biomarkers is exactly what the NIH declined to spend its squillion dollars on. Oddly.
[4] Dry, very dry.


There is no altruism in scientific publishing, much of which has become a Slough of Despond. The shoutout to Nature, Science, JAMA et al. is well deserved!
This is exactly why so many of us urged you to continue your laborious coverage. Many thanks!
Agree wholeheartedly with judy sixbey.
I will forward this post to a medical doctor friend who seems to have become resigned to repeated reinfection.
—
It is disheartening that MSM does not seem to be interested in this. One would think that their business model requires some minimum level of health in the population, and some maximum level above which the prevalence of disability must not rise, in order for there to be enough of a market for their “information products” that is able to pay to fund their enterprises.
It seems to me that intentional disregard of stories like this is self-defeating from the standpoint of future business operations.
—-
‘ I’ll be gone, you’ll be gone ‘: classic short-term thinking that in the context of the CV pandemic seems likely to take on the character of ‘self-fulfilling prophecy.’
Thank you, Lambert, for the continuing covid coverage. Save a handful of Twitter follows (who I couldn’t check in on during the recent Elon-imposed outage), NC is the only place remaining that one can turn to for covid news.
On a totally unrelated note, I went to the doctor today for a long-overdue physical which I had been putting off for the last couple of years for some reason. I was the only person wearing mask, of course.
They were worried about my cholesterol being slightly elevated but didn’t want to do anything to prevent me (or themselves) from catching a contagious illness that is now proven to increase the risk of heart attack…
The only place. Incredible. I mean I believe it.
>If 10% of acute infections lead to persistent symptoms, it could be predicted that ~400 million individuals globally are in need of support for long COVID.
This assumes everyone only gets Covid once which is obviously incorrect. The more reasonable prediction may well be orders of magnitude more
We must never forgot. This can all end with six months of social provisioning and two months true quarantines, plus some ongoing inconvenient for international travelers perhaps forever, along with universal masking in some environments and free testing and probably random testing at hospitals and schools.
This can all end.
But markets.
You’ve got my vote.
Well, it can stop getting worse (and that is earnestly to be desired).
The “baked in” damage from 3+ years of failure to take these measures will not go away, and it will be interesting to see whether there will be much in the way of social provisioning for those who are no longer able to sustain themselves through sale of their labor.
I’m not optimistic that we will avoid slow system collapse (sort of an economy-wide analogue of what seems likely to happen to individuals as they rack up annual or more frequent than annual infections.)
What about animal reservoirs? There are a lot of rats and cats and deer.
This is exactly why the failure to do everything to stop transmission during the first 6 months or so of the pandemic (except in a few countries) is so ominous.
Covid-19 is now endemic, just like, say, malaria — except probably worldwide, unlike malaria. Eradicating the coronavirus requires not just setting up the whole gambit of masking, testing, filtering, quarantaining, curing, and supporting people economically and regarding activities such as education in human societies, it also requires a daunting environmental screening, containment, and probably culling of animal reservoirs, some of which (e.g. rats) are almost impervious to complete control.
The magnitude of organizational skills, technical resources, personnel, long-term perseverance, and of course cost, ensure that this will not even be seriously attempted under the prevaling political and ideological conditions.
But what about “personal risk assessment”?!
Health authorities worldwide provide maps of countries and regions where malaria is endemic, with advice on which prophylactic is effective (depending on the malaria strain). One also uses mosquito nets and insect repellants.
With covid, authorities no longer even bother publishing accurate statistics on time, there is no effective prophylactic, one must fabricate one’s own equivalent of insect repellant (Corsi-Rosenthal boxes), and in a disturbing number of cases, using the equivalent of a mosquito net (FFP2 masks and better) is discouraged, or even prohibited.
Ergo: not only are we hampered when assessing personal risks, we are even hindered in taking our own precautions.
I’d considered that, and I’d say it’s better to try and fail than to not even bother; I think having any kind of country to salvage morally simply demands it, even in failure. Maybe it’s impossible to prevent sufficient animal transmission to humans for there to be any viable strategy going forward, but it probably isn’t possible to know unless we try.
I’d rather not kill large numbers of animals on speculation. Anyway, we won’t do so; our brains will be too far gone to organize anything like that.
Regarding the subject of rabies for example, vampire bats can prey on cattle.
And then you have: “SARS-CoV-2, the virus that causes COVID-19, has been detected in cats, dogs, rodents, deer, apes and a variety of farm and zoo animals. It can also mutate in these animal hosts, leading to new variants.” https://www.upi.com/Science_News/2023/07/10/all-species-COVID-19-test/9051688999414/
I wouldn’t advocate knocking off bats in general due to impacts on insect populations (more insects). However, if a SARS-CoV-2 variant goes through a cattle herd, and vampire bats pick it up…aren’t bats one of the primo mutators of viruses on the planet? [deja vu, right?] Not to scare folks, but the facts someday might wake up TPTB? In the future it might not be a good idea to drive down bovine or porcine immune systems on industrial farms?
Not even industrial. “They did, however, find reductions in infection rates when the ranchers culled bats prior to detecting infections in their herds.” https://phys.org/news/2023-03-culling-rabies-outbreak-ineffective-strategy.html
I don’t see reference to the effects of covid after getting the vaccine. The second shot just nailed me and I have the symptoms of Long Covid. Im I the only one or is it just not included in the reports?
Here’s an article on that topic: https://www.science.org/content/article/rare-link-between-coronavirus-vaccines-and-long-covid-illness-starts-gain-acceptance
It was the sixth shot (yes, I’m quite afraid of getting Covid-19) that got me. Knocked me down for three days. Not sure if there have been any long lasting effects because I already have ME/CFS and am nearly as old as Biden, so I’m not sure I could tell.
Thank you so much Lee. After two years I’m a lot better but still lethargic.
I can’t seem to post links from my phone, but the Twitter of @vijayiyer312 might be of interest to you.
My impression from the reading I’ve done (and that’s all it is, just an impression) is that severe vaccine injuries probably usually involve some sort of predisposition in the patient – genetics plus prior infections and/or endogenous viruses, those sorts of things. Note that, far from exculpating the vaccines and their manufacturers, any such factors that are found will serve to indict the trials and approval process as inadequate at best. I suppose it might really be true that nobody could have guessed, but I was guessing similar things back in 2020.
From the second study:
“Notably, no significant differences were noted in the incidence of long COVID at 24 months in terms of the number of vaccinations received.”
Yeah, if I had a nickel for everyone who told me “I’m getting the booster because I’m afraid of long covid and it might help.” It was a thing.
I’m finding this part a bit confusing. Subjects’ infections occured early in 2020? Would this be vaccination-as-treatment?
There was such an idea once upon a time — that vaccination will help resolve existing LongCOVID
Off topic…are there any accounts of people avoiding the bug until omicron gave them what they thought was a wicked wicked nose-throat-ears strep throat? And then having prior back problems get worse PLUS, for instance, Pseudo gout and Sjogren’s syndrome…all at once? I was suspicious about the throat thing, but at the time my test was negative.
Yesterday, I ran into to a neighbour who I hadn’t seen for a few weeks. She had temporal arteritis which is perhaps caused by a faulty immune system response. Treated in hospital, 3 inch scar on her forehead where they removed a piece of damaged artery. Can be fatal if not treated promptly. https://my.clevelandclinic.org/health/diseases/15674-temporal-arteritis
She is 75ish, vaxxed to the max, has never had a symptomatic case of COVID. Could there be a link re the many vaccines? Unclear, the condition is not common but generally hits those over 50. What is clear is that no one is asking. I found an article about increase in cases from 2000-2018 in Ontario but not seeing any recent I.e pandemic related research.
I am glad to see the long COVID research coming out. And many thanks to Lambert for keeping us abreast of it. I do wonder if many doctors/researchers are tracking unusual increases in incidents of disease over the course of the pandemic. I have friend whose has a rare (uveal) melanoma that has metastasized in her liver rather more quickly than it often does. She has had COVID twice (frequent flyer to visit family), not sure about her vaccine status but know she has had at least a couple. If our T cells are affected by this disease, then surely cancer rates are increasing?
Here is A Midwestern Doctor’s take on your concerns,
https://igorchudov.substack.com/p/cognitive-impairment-in-adults-what?publication_id=441185&post_id=134425752&isFreemail=true
His take is both Covid-19 and the vaccines can cause these symptoms.
At what rates?
Lambert you’re a lifesaver. I’m sending my progeny a link to this instead of the harangue I had intended. Much less stressful. Many thanks!
I have an 81 y.o. friend who is an academic scientist who has been reading Nature forever. I was over at his place (outside) a couple of days ago. He told me that some Nature articles had come out re long covid and it looked to him like it was becoming less of a problem. As far as I can tell he is still smart and has not become demented, but there is something that is happening to people’s brains.
Thank you for continuing to cover this. And thank you for not catching covid. Partly for your own sake, and partly because I fear that if you do, you will lose the ability to see what is happening.
Oh dear. I’ve only skimmed the material, but I suspect his limbic system is editing what his intellect gets to read, so to speak.
It can happen to the best of us, or so I tell myself, since it has definitely happened to me.
Yes, I think that is right. I have read the older a person gets, the better s/he typically gets at not focusing on horrid things. I see that in my elderly relatives and friends; the bad stuff just doesn’t stick in their brains, no matter how smart they are. That is a real problem if you are hoping to get people to avoid catching covid.
I’m closing in on 60 so I am still young enough to focus relentlessly on the miserable stuff.
So I was texting a friend about this article and as I was typing in “long covid” and it autosuggested “king Covid.”
If you guys at NC would get with the 20th Century and add a “like” button then I wouldn’t have to actually write out another Thank You!
The conclusion I draw is that editors at the NYT, WSJ, WaPo, Salon, and all the other outlets Lambert mentioned — they have all been persuaded by “the science” that this is yesterday’s news and that “we need to move on”.
Thank you so much, Lambert! This is why we LOVE this family-blog Family Blog!
Thank you Lambert, this is a genuine public service. Since my lurker access Twitter was cut off, I’m missing crucial updates on COVID, so this and other coverage by NC help to fill the gap.
Concur with all above Lambert.
This sort of pain staking attention to detail, reconciling past and present, makes you invaluable to NC and its readership. More so, as noted above, provides a linkable post which readership can forward to others, which then negates the verbal issues with discussing a topic with those that have gifted biases or some other malady which makes discussions difficult.
Well done Sir ….
Out of morbid curiosity. I just googled «long covid nature» to see if any MSM ‘news’ sources had picked up on Nature’s salvo. Three pages down I got my first hit:
https://www.nakedcapitalism.com/2023/07/this-week-in-long-covid-nature-fires-salvo-four-major-papers.html
Lambert truly is our indispensible news source.
It certainly appears that since Biden declared that Covid is no longer, the MSM haven’t taken the cue and erased it entirely. In fact, health care as a general source of misery for almost every American family has disappeared from their pages. You used to read about it fairly often, and now it’s just gone, clearly because the Democrats have no meaningful policy initiatives, so it’s best to just forget about it entirely. And they can’t figure out how to blame Trump or the Russians. So it’s just more MSM normalizing of the struggle of everyday American life, as they ask people to stretch their cognitive dissonance until their heads begin to crack.
This