By Lambert Strether of Corrente.
Respiratory viruses[1] are much in the news. We are said to be in a seasonal “tripledemic” of the Flu, RSV, and Covid (even though Covid is not really seasonal[2]). I’ll lay the groundwork by first defining the diseases that make up the “tripledemic,” and then discuss the tripledemic itself (special guest appearance by Leana Wen!). I will then present the conventional wisdom for Flu and RSV transmission: droplet dogma — “that transmission of respiratory diseases is caused by large droplets, and thus, droplet mitigation efforts would be good enough”– with a dash of fomites[3]. I will then show that both RSV and the Flu are transmitted via airborne aerosols (“spread like smoke”), just like Covid, first by discussing respiratory virus transmission generally, then by discussing the individual viruses. For you, dear readers, this is important: If you have a layered protocol for avoiding Covid based on airborne tranmission — perhaps including masks, ventilation, filtration, various sprays, and the avoidance of 3Cs spaces — that protocol will help prevent RSV and the flu as well. It’s a three-fer. Now let’s define our three viruses.
RSV is a “negative-sense, single-strand, enveloped RNA virus.” CDC explains:
Respiratory syncytial (sin-SISH-uhl) virus, or RSV, is a common respiratory virus that usually causes mild, cold-like symptoms. Most people recover in a week or two, but RSV can be serious. Infants and older adults are more likely to develop severe RSV and need hospitalization.
The Flu. “All influenza viruses consist of single-stranded RNA as opposed to dual-stranded DNA… [T]wo influenza types (A and B) that cause seasonal epidemics.” CDC explains:
Flu is a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and sometimes the lungs. It can cause mild to severe illness, and at times can lead to death.
Covid. “Coronavirus (CoV) genomes consist of positive-sense single-stranded RNA and are among the largest viral RNAs known to date.” CDC explains:
[Covid-19] can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States. COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs and respiratory system. Other parts of your body may also be affected by the disease. Most people with COVID-19 have mild symptoms, but some people become severely ill. Some people including those with minor or no symptoms will develop Post-COVID Conditions – also called ‘Long COVID.”
(Note that the detail of CDC’s description for Covid suggests that “one of these three is not like the others”).
Now to the tripledemic. From Yale Medicine:
There’s no scientific definition for this term; it simply refers to a collision of RSV (respiratory syncytial virus), flu, and COVID-19 to the extent that it might overwhelm hospital emergency departments.
No “scientific definition,” therefore, I suppose, public relations; the origin of the term not clear, it it became current in October 2022, “wafting through social circles and making rounds in the news cycle” (like so many other words, including “herd immunity,” “immunity debt,” and “mild”). Here is a usage example from the Chicago Tribune, “‘Tripledemic’? Local medical experts urge vaccination as COVID, flu and RSV hospitalizations spike nationwide“:
Medical experts are also alarmed by a simultaneous rise in recent hospitalizations for other respiratory illnesses like RSV and the flu, with the CDC issuing an “urgent need” to raise vaccination coverage against all three viruses nationwide.
In anticipation of the coming holiday gatherings, which tend to increase the spread of respiratory viruses, local physicians are encouraging the public to get all vaccinations they’re eligible for, including the updated COVID booster shot, which targets currently circulating strains of the virus.
Notice that both Yale and the Chicago Tribune are hospital-centric (madness, when you consider that even a mild case of Covid can cause brain damage). Notice also that the “medical experts” are focus entirely on vax; no non-pharmaceutical interventions are mentioned. CDC does a little better, but not much. Here is their “Health Advisory” of December 14, “Urgent Need to Increase Immunization Coverage for Influenza, COVID-19, and RSV and Use of Authorized/Approved Therapeutics in the Setting of Increased Respiratory Disease Activity During the 2023 – 2024 Winter Season“:
The Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to alert healthcare providers to low vaccination rates against influenza, COVID-19, and RSV (respiratory syncytial virus).
Healthcare providers should also counsel patients about testing and other preventive measures, including covering coughs/sneezes, staying at home when sick, improving ventilation at home or work, and washing hands to protect themselves and others against respiratory diseases.
No mention of masks, of course; Mandy won’t have that. No mention of filters, for that matter. And implicit support for droplet dogma (“covering coughs/sneezes”) and fomites (“washing hands”). So another dog’s breakfast from CDC.
I can think of no pundit better equipped to summarize the state of play on the tripledemic than Sociopath of the Day Leana Wen, interviewed yet again on the teebee:
As respiratory viruses spread everywhere, what should you do if you get sick?
Again, for most people, it’s not important to know exactly what is causing their symptoms. The treatment is generally the same and is referred to as supportive treatment. That means there is no specific antiviral therapy, but rather, symptoms are addressed to help the patient feel better. So, if someone has a fever, they can take fever-reducing agents like Tylenol or ibuprofen. They can drink lots of fluids to prevent dehydration. They can get rest to help with their fatigue. That’s different in the case of influenza and Covid-19 for specific patients who are eligible for antiviral treatment; those are the people for whom testing is most crucial.
And by “eligible,” we mean “economically eligible,” of course. The subtly sociopathic point here is that Wen is really saying that your subsequent behavior after showing symptoms should be the same: It doesn’t matter whether you infect your grandmother with Covid or with the Flu. This is minimization on the grand scale!
Having defined our three respiratory viruses, and the “tripledemic” into which they have somewhat arbitrarily been dumped, let’s turn to modes of transmission. Conventional wisdom here for RSV and the Flu is shaped by “droplet dogma,” which assumes that transmission takes place via large droplets (“loogies” produced by coughing or sneezing, and certainly not by mere breathing). I will assume that droplet dogma has been defeated and replaced by aerosol transmission in the world of science — which most definitely does not include Hospital Infection Control — but for RSV and Flu, droplet dogma remains virtually unassailed. Let’s look at RSV and then the Flu. (I have to quote multiple sources so you can see how pervasive droplet dogma is.)
Droplet Dogma: RSV
From the CDC:
RSV can spread when
- An infected person coughs or sneezes
- You get virus droplets from a cough or sneeze in your eyes, nose, or mouth
- You have direct contact with the virus, like kissing the face of a child with RSV
You touch a surface that has the virus on it, like a doorknob, and then touch your face before washing your hands
As you can see, droplet dogma with fomite topping, as are the next two examples.
From the New York State Department of Health:
RSV is spread through contact with droplets from the nose and throat of infected people when they cough and sneeze. RSV can also spread through dried respiratory secretions on bedclothes and similar items. Direct contact with the virus, such as kissing, can also spread the virus. RSV can remain infectious on hard surfaces for several hours and on skin for shorter amounts of time.
And from UCHealth:
RSV is contagious as it is airborne. RSV spreads much like COVID-19, through virus droplets that enter the body through the eyes, nose or mouth. People can get RSV through direct contact, like kissing a child’s face who has RSV. The virus also can survive on hard surfaces for many hours. It survives on soft surfaces for a shorter amount of time.
Similar to precautions someone would take if they had the flu or COVID-19, people with RSV are contagious and should stay home and away from other people to avoid spreading the virus. Wash your hands often and avoid touching your eyes, nose or mouth with unwashed hands as this is how germs spread. Cover your cough or sneezes with your elbow or with a tissue, tossing it in the trash when you are done. Disinfect and clean frequently used surfaces to avoid spreading germs.
Notice that by accident or malice, UChealth has snuck in the word “airborne” (which is literally true, I suppose, in the sense that when you hack up a loogie, it flies through the air. There is no sense that RSV is an aerosol, however, that “spreads like smoke.” All the rest of their verbiage is entirely consistent with droplet and fomite transmission.
Droplet Dogma: The Flu
From the CDC:
Most experts believe that flu viruses spread mainly by tiny droplets made when people with flu cough, sneeze, or talk. These droplets can land in the mouths or noses of people who are nearby. Less often, a person might get flu by touching a surface or object that has flu virus on it and then touching their own mouth, nose or possibly their eyes
Droplet dogma with fomite topping. There is no suggestion, for example, that the Flu might be spread by breathing.
From the New York State Department of Health:
The flu is caused by a virus and spread mainly by coughing, sneezing or close contact.
The same. (Note that “close contact” is, by itself, not a mode of transmission. Close contact means what? Touch? Shared air? Sneezing and coughing? Little infected elves?)
And from Johns Hopkins:
The flu virus spreads mainly by droplets when infected people cough, sneeze, or even talk, but it can be spread by touching surfaces on which one of those droplets has landed and then touching one’s nose, mouth or eyes.
The same.
About Droplet Dogma
Readers will be familiar with the battle to change the paradigm of Covid transmission from droplet dogma to airborne aerosols, won on the science, and not yet won in the institutions (see NC here, here, here, and here). It took real scholarship and a gift for polemic to straighten out the infection control community on their outmoded paradigm, and in the meantime, droplet dogmatists killed a lot of innocent people. From Jimenez, et al., “What were the historical reasons for the resistance to recognizing airborne transmission during the COVID-19 pandemic?”
Just as the COVID-19 pandemic was getting started, Chen et al. reported that “Reviewing the literature on large droplet transmission, one can find no direct evidence for large droplets as the route of transmission of any disease.” One of the earliest reports about the early outbreaks in China in the prominent Nature journal concluded that “the disease could be transmitted by airborne transmission, although we cannot rule out other possible routes of transmission.” Some early public health announcements in China reported that the novel coronavirus was airborne. However, and despite a lack of direct evidence in favor of droplet or fomite transmission, by March 2020 public health institutions like WHO concluded that ease of transmission in close proximity proved that COVID-19 was transmitted by those mechanisms…. The very slow and haphazard acceptance of the evidence of airborne transmission of SARS-CoV-2 by major public health organizations contributed to a suboptimal control of the pandemic, whereas the benefits of protection measures against aerosol transmission are becoming well established.
“Suboptimal” is good. So, let’s not make, or continue to make, similar mistakes in course of the tripledemic. Let’s now present evidence that those diseases, too, are spread by airborne tranmission. First, I’ll show that respiratory diseases generally are spread by airborne aerosols. Then, I’ll look at the specific cases of the Flu and RSV.
Respiratory Diseases Are Spread by Airborne Aerosols
Here are three sources, ordered by increasing strength.
First, from the Covid is Airborne site, this table organizes studies that give evidence supporting airborne transmission by disease:
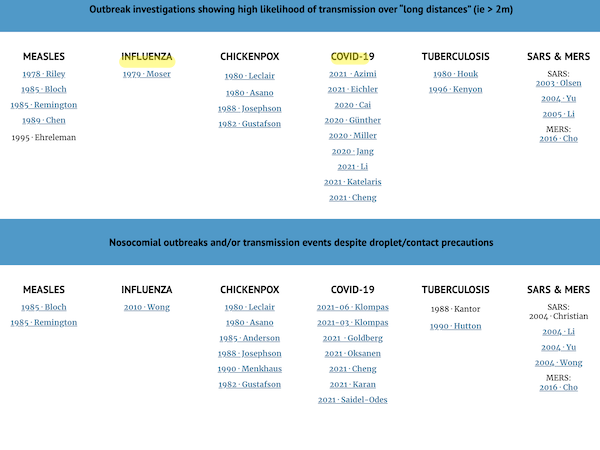
I wish there were column for RSV, but the tabular format is really great, suitable for gifted amateurs like us to propagate on the Internet.
Second, from Tang et al., in Indoor Air: “Hypothesis: All respiratory viruses (including SARS-CoV-2) are aerosol-transmitted,” a review of the literature:
So how are these various viruses spread? The hypothesis being presented here is that all of these viruses are spread via aerosol transmission (including short-range aerosol transmission). There are several consequences to this if this hypothesis is accepted. For example, if aerosol transmission is accepted for any one of these seasonal respiratory viruses, such as SARS-CoV-2, then this has implications for infection control practices including the choice of PPE, masking in the community setting, and social distancing. Improved ventilation indoors, in both the community and healthcare settings, will reduce the transmission of all of these viruses, as has already been reported, due to the global impact of various non-pharmaceutical COVID-19 interventions
Evidence to support aerosol transmission comes in several forms, including from outbreak investigations, direct environmental and near-patient air sampling, as well as mechanistic arguments and models validated with real-world data.
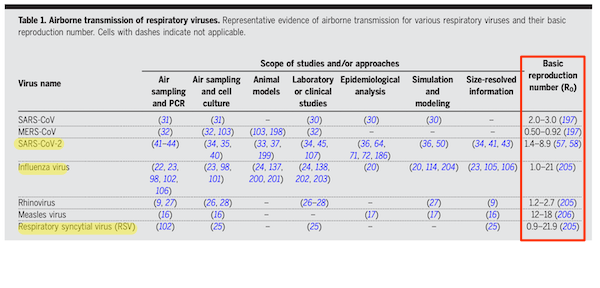
Third, from Wang et al., Science: “Airborne transmission of respiratory viruses“:
Despite the assumed dominance of droplet transmission, there is robust evidence supporting the airborne transmission of many respiratory viruses, including measles virus, influenza virus, respiratory syncytial virus (RSV), human rhinovirus (hRV), adenovirus, enterovirus, severe acute respiratory syndrome coronavirus (SARSCoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and SARS-CoV-2. Airborne transmission has been estimated to account for approximately half of the transmission of influenza A virus in one study of a household setting. A human challenge study on rhinovirus transmission concluded that aerosols were likely the dominant transmission mode.
They provide a handy table, especially useful because it contains the R0 values in the rightmost column:
Now let’s turn to the individual viruses.
RSV Is an Airborne Aerosol
From the American Journal of Respiratory and Critical Care Medicine, “Evidence of Respiratory Syncytial Virus Spread by Aerosol. Time to Revisit Infection Control Strategies?”:
Objectives: To determine if the air surrounding infants with RSV-positive bronchiolitis contains RSV in aerosolized particles that remain capable of causing infection.
Methods: The amount of RSV contained in aerosolized particles produced by infants with bronchiolitis due to RSV was measured using viable impactor sampling. The ability of RSV contained in these particles to infect healthy and chronic obstructive pulmonary disease (COPD) human ciliated respiratory epithelium was determined.
Results: We showed for the first time that infants with RSV-positive bronchiolitis nursed in a ward setting or ventilated in intensive care produced large numbers of aerosol particles containing RSV that remained infectious and were capable of infecting healthy and COPD human ciliated epithelium. A significant amount of RSV was found in particles with aerodynamic diameters less than 5 μm.
Conclusions: Many of the aerosolized particles that contained RSV in the air surrounding infants with bronchiolitis were sufficiently small to remain airborne for a significant length of time and small enough to be inhaled and deposited throughout the respiratory tract. It is likely that this leads to spread of infection to others, with dissemination of infection throughout the respiratory tract.
From 2015, sadly. Dogma takes a long time to jackhammer.
From the European Respiratory Journal, “Airborne transmission of respiratory syncytial virus (RSV) infection“:
18 infants with “RSV Bronchiolitis” were recruited. An Andersen microbial impactor was placed 100cm from the head of the patient and run for 30min fractionating collected particles into different aerosol size distributions. Room air was impacted into 20ml of RPMI growth media and its infectivity of A549 was determined using plaque assays. Immunofluorescence staining of the infected A549 cells was used to confirm RSV infection.
Results: 17 infants produced infectious airborne particles less than 4.7μ. We estimated the number of infectious RSV within aerosols of less than 4.7μ produced from 12/17 patients to be 188.5±68 (mean ± SEM, range 2.4 to 4044) in 10 litres of air. This volume would be inhaled by a 3.1kg baby in 10 minutes (respiratory rate 40/min; tidal volume 8ml/kg).
Conclusion: Infants with RSV bronchiolitis produce aerosols that contain infectious RSV in aerosols small enough to deposit in the lower airways. These findings may influence infection control strategies to prevent aerosol transmission of RSV in a hospital setting.
From 2011. Ditto.
The Flu Is an Airborne Aerosol
From Viruses, “Influenza A and B Viruses in Fine Aerosols of Exhaled Breath Samples from Patients in Tropical Singapore“:
Although air sampling has demonstrated the presence of influenza virus RNA in the air of healthcare settings, very little is understood about the potential of such infectious agents to be produced and transmitted directly from human respiratory activities. Various experiments have attempted to capture some of the droplet populations generated by various activities. However, many of these droplets were lost due to settling onto unsampled surfaces, or because only specific droplet parameters were measured. In this study, we utilized a high-efficiency particulate breath collector (G-II) to capture most of the exhaled aerosols during tidal breathing. We detected influenza virus RNA in the fine (42%) and coarse (29%) fractions of subjects with laboratory-confirmed influenza.
Assuming a conservative estimate of 3 TCID50, this suggests that a 0.7 s exposure (to the highest emitter) to a 3.5 h exposure (to the lowest emitter) to the fine aerosols of an infected individual from our study could result in an infection in 50% of the population.
In conclusion, this study has shown that aerosolized influenza virus is detected mainly in the fine aerosol fraction from natural patient breath and exhibits infectivity in nearly one-third of subjects.
RSV and Flu Are Airborne Aerosols
Here is a study for both! From Clinical Infectious Diseases, “Distribution of Airborne Influenza Virus and Respiratory Syncytial Virus in an Urgent Care Medical Clinic“:
Airborne particles were collected in an urgent care clinic with use of stationary and personal aerosol samplers. The amounts of airborne influenza A, influenza B, and RSV RNA were determined using real-time quantitative polymerase chain reaction. Health care workers and patients participating in the study were tested for influenza.
Airborne particles containing influenza and RSV RNA were detected throughout a health care facility. The particles were small enough to remain airborne for an extended time and to be inhaled deeply into the respiratory tract. These results support the possibility that influenza and RSV can be transmitted by the airborne route and suggest that further investigation of the potential of these particles to transmit infection is warranted.
(“Throughout a health care facility” is, of course, an argument for universal masking.) From 2010, ditto.
Conclusion
What I like about all the above studies is that they’re actually sampling the air; we’re not talking models, or (heaven forfend) meta-studies. Just a final word of debunkment on coughing and sneezing. Often, when coughing and sneezkng are treated as the main modes of tranmission, people are recommended to cough or sneeze into their elbows, or cover their mouths (“cough etiquette”). But see from BMC Public Health, “Effectiveness of cough etiquette maneuvers in disrupting the chain of transmission of infectious respiratory diseases“:
In this study, 31 healthy non-smokers performed cough etiquette maneuvers in an effort to cover their voluntarily elicited best effort coughs in an open bench format. A laser diffraction system was used to obtain accurate, non-invasive, quantitative, real time measurements of the size and number of droplets emitted during the assessed cough etiquette maneuvers.
Recommended cough etiquette maneuvers did not block the release and dispersion of a variety of different diameter droplets to the surrounding environment. Droplets smaller than one-micron size dominate the total number of droplets leaked when practicing assessed maneuvers.
All the assessed cough etiquette maneuvers, performed as recommended, do not block droplets expelled as aerosol when coughing.
Of course, I’m not recommending that you cough or sneeze on people, or stop washing your hands, or fail to clean surfaces. Heaven forfend! Nor can I entirely rule out, for RSV and the Flu, fomite and large droplet tranmission, even if the main evidence for the latter seems to be the stubbornness of reactionary dogmatists. However, ignoring that all three respiratory viruses — Covid, RSV, and the Flu — spread through airborne aerosol transmission is medical maleficence, bordering on criminal. Why would we not want to protect people in all possible ways? And do note the good news: Your personal protocol of layered protection for Covid scales to help with RSV and the Flu, as well[4]!
NOTES
[1] From Indoor Air, “Hypothesis: All respiratory viruses (including SARS-CoV-2) are aerosol-transmitted“:
Respiratory viruses do not have a strict definition. In the simplest sense, they are viruses that can be inhaled into the respiratory tract (URT), where they can replicate and cause a variety of respiratory syndromes including common colds, croup, cough and fever, bronchiolitis, and pneumonitis. They can also be expelled from the respiratory tract in exhaled breath as virus aerosols, as has been demonstrated in naturally-infected volunteers or air-sampling studies from hospital settings, for several respiratory viruses, including influenza, respiratory syncytial virus, coronaviruses, and rhinoviruses.
[2] From Wired, “Why It’s Too Soon to Call It Covid Season“:
[E]xperts on the front lines and doing data analysis say it’s too soon to declare that Covid has achieved seasonality. Looking back over the previous three years, they do see patterns: a spike at some point in the summer, such as the arrival of the Delta variant in 2021, and a spike sometime in the late fall or winter, such as the Thanksgiving surge of Omicron later that year. But those spikes haven’t occurred at the exact same time from year to year, and it’s possible they didn’t all arise for the same reasons.
“You might look at that data and think, maybe this is just a biannual virus, compared to flu and RSV, which have single seasonal peaks,” says Cameron Wolfe, an infectious disease physician and professor at the Duke University School of Medicine. “But that gets much harder to say when you factor in that as a society we behave very differently, seasonally. And that we’ve behaved differently in different years of the pandemic, according to how restricted we were in terms of our movements, how much mitigation we were actually performing, and how immune we were, either by vaccine or native infection.”
In other words, what looks like a season might be an artifact created by our behavior, not the virus’s. The way our bodies react to SARS-CoV-2 might also be playing a role in pushing it around the calendar.
The urge to stuff Covid, RSV, and the Flu into the same box as “seasonal viruses” seems strange and not based on science. I’m guessing there are two drivers: Covid minimization (“it’s just the flu”), and the fact that there’s an entire institutional apparatus already devoted to seasonal viruse — PR, treatment, vaccination — so why not give that apparatus the Covid file?
[3] I do not claim that the flu and RSV are not spread by fomites and loogies large droplets; rather that they are spread by airborne aerosols, in addition to these other putative modes of transmission, for which the evidence is bad, though the dogma be strong.
[4] Not sure about sprays and mouthwash. Seems reasonable, but I’d want evidence. Readers?


Interesting, the Chinese are working on a dry-powder inhaled vaccine platform to induce mucosal blocking or immunity of airborne viruses:
https://www.globaltimes.cn/page/202312/1303620.shtml
December 14, 2023
Chinese researchers develop novel dry-powder inhaled vaccine technology; study * published in Nature
By Liu Xin
https://www.globaltimes.cn/Portals/0/attachment/2023/2023-12-12/64085f1e-f185-4397-801e-4ea480a90d4e.jpeg
Researchers from the Institute of Process Engineering (IPE) of the Chinese Academy of Sciences have proposed a new “nano-micro composite” delivery concept for vaccines and developed a single-dose, dry-powder, inhalable vaccine platform. The vaccine made in the laboratory based on the technology is effective in blocking respiratory viral infection and transmission in animal tests, showing great promise for combating future emerging and epidemic infectious diseases. This study was published in Nature on Wednesday….
* https://www.nature.com/articles/s41586-023-06809-8
Thank you for aggregating all of these studies, Lambert. A very impressive bit of work!
After March 2020 things will never be the same.
The BNSF line (west burbs) had daily ridership of 65,000 4 years ago. Now it’s 16,000. WFH for the win! Fewer diesel trains, less climate change exposure. No Me Too workplace employers liability insurance claims.
Would be great if James Burke of Connections PBS series discussed.
I have been to so many places (supermarkets, clinics, hospitals, restaurants etc) where there are hand sanitizers provided but no one wears a mask and there is no visible effort to provide proper ventilation. It’s nuts.
The great thing about hand sanitizers is that hardly anybody uses them, so the maintenance cost is near zero. Replace the plastic pouch of goo once a year or so.
I see the hand sanitizers in every store here in Europe as well. They’ve become Covids rainbow flag. Businesses put a hand sanitizer at their entrance as a “show of their support”, a meaningless gesture that symbolizes “We’re with …”. I wonder how these businesses would react if people started adding other symbols to the hand sanitizers, like hanging rainbow flags, Ukrainian flags, Israeli flags and yellow ribbons on the hand sanitizers. Just bomb these stores with all of their other meaningless gestures in one place to make a point of how superficial and hypocritical their “show of support” really is.
Because sanitizing hands is your responsibility, while doing something about ventilation or masking would be somebody else’s responsibility. Neat trick, that.
It’s also a lot cheaper.
Thanks as always, Lambert! Great work.
I think nasal sprays and mouthwashes are valid means of intervention. Nasal sprays are superior because they can directly neutralize (if virucidal) any virus present around the epithelial cells/surfaces that are most susceptible.
Mouthwashes will protect/disinfect areas in the mouth and further down the pharyngeal tract where the virus will naturally get shed as a result of breathing.
#SwissCheeseFTW
What Wen says isn’t even true. If you’re infected with SARS 2 you can get Paxlovid if you’re a believer in Pfizer. So she’s wrong even hailing from vax and relax land. So much for the tools when even this tool erases a tool. Got it?
Also recent news about long flu:
https://medicine.wustl.edu/news/long-flu-has-emerged-as-a-consequence-similar-to-long-covid-19/
Etc.
https://www.globaltimes.cn/page/202312/1303823.shtml
December 17, 2023
Chinese scientists published first study on long COVID at 3 years after primary infection
Chinese scientists have published the first study on long COVID three years after the primary infection.
According to the latest study jointly conducted by teams led by Cao Bin from China-Japan Friendship Hospital and Zhang Dingyu, head of Wuhan Jinyintan Hospital, approximately half of COVID-19 survivors exhibited at least one sequelae symptom after three years from the onset of symptoms.
The most prevalent long COVID symptoms reported were fatigue or muscle weakness, and hair loss. The study, * published in The Lancet’s respiratory medicine version on December 21, noted that compared with survivors without long COVID, those with long COVID had a higher proportion of re-infection and were more prone to pneumonia after re-infection….
* https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(23)00684-9/fulltext
Or you can stay home. God forbid the mandated mask requirements of 3 years ago. Thanks but no thanks.
Indeed, that’s what I do, because when I go out, I meet so many [glass bowls]. It gets tiring. Kidding!
I may have written this anecdote in the comments before. Nevertheless, let me relate my super sensory ability to aerosols.
I am greatly annoyed when I have to go to a crowded place to get something important done, and nobody is wearing a mask to protect me. I tend to wear a respirator if I know I will not be doing much talking, e.g. grocery shopping. I “downgrade” to an N95 if the situation demands I speak, e.g. non-ATM bank services. One inadvertent benefit of my mask wearing is I don’t suddenly get hit by a wave of odor. It is quite useful for me to wear a respirator, and I don’t have to worry about sudden unpleasant odors disturbing me from my current task. I really do not want to smell laundry detergent, perfume, or deodorant emanating from a crowd of people. I must avoid cigarette smoke like the plague. If you smoked a cigarette three days ago, I can probably still smell it. Another unfortunate aspect of my super nose is I can not discern the direction of the odor, unlike dogs. If I smell cigarette smoke, my solution is to hold my breath and head the other direction, but I don’t really know which direction is the other way is until I can visually see somebody smoking. If a single smoker is actively smoking outdoors, I can usually spot it quickly. If a smoker finishes his business and is in a room with others, I can still smell the third hand smoke, but I don’t have the capability to distinguish who is causing my distress.
Lambert’s post above and a great paper I found on PNAS somewhere hypothesizes about the particle size of SARS-CoV-2 as being similar to cigarette smoke particles. Specifically, the larger virus particles tend to be droplets, and the smaller virus particles tend to aerosolize. Perhaps other commenters here can offer insight on the inclination of SARS-CoV-2 to aerosolize and its ability to use the mucus of hosts.
Nevertheless, let me return to my super nose anecdotes. I was wearing an N95 mask in an empty waiting room at the doctor’s office, and a smoker enters the clinic. He, maskless, checks in at the front desk, and I can smell cigarette smoke through my N95 mask 3-5 minutes after he entered. The smoker had enough time to check in but not enough time to walk towards the waiting room, and his cigarette aerosols filled the room in minutes. I have enough experience with wearing respirators that I can confidently predict it would have taken 15-25 minutes for me to smell the cigarette odors if I were wearing a respirator. The implications of this as it relates to SARS-CoV-2 aerosols are ruinous, especially if other measures to curb its transmission are not taken.
From the largest hospital on Vancouver Island, working Sunday, I had a request to do a portable exam on a really sick old man. We couldn’t do the exam after a couple attempts due to he was being intubated, then moved to a different dept, then moved to ICU. He’d had several CT exams that same morning so I asked the radiologist to look at them and see if we could narrow the exposure and focus the exam. While looking thru the chest CT the rad said “this pt has covid pneumonia”. Been a long time since we heard that diagnosis. Going to be a long winter.
China spent $21 billion on Covid prevention this year, much of which went to upgrade hospitals’ ventilation and air sterilization. Seems to be money well spent.
This all gives me anxiety just thinking about it again. That was a good read though whomever suggested it.
https://medicine.wustl.edu/news/long-flu-has-emerged-as-a-consequence-similar-to-long-covid-19/
Nasal vaccination not complying with hope: https://pubmed.ncbi.nlm.nih.gov/36229342/