By Lambert Strether of Corrente.
Readers, there are two UPDATES, the first knocking out footnote 6 in the evidentiary review section, the second showing that hospital fears of liability over SARS-CoV-2 infection were not unfounded, since now a personal injury lawfirm is seeking clients to sue them for it.
I apologize in advance for this book-length, grab two-cups-of-coffee post, but I think that empowering the Covid-conscious by maximizing the attack surface for assaults on the CDC’s Hospital Infection Prevention and Control Advisory Committee (HICPAC)’s anti-mask, anti-science infection control “Guidance”[1] (“CDC Advised To Weaken Infection Protections As Mysterious Pneumonia Brews Overseas“) is important, tactically, just now, and so I’m gathering as much information as I can, here, in one place. And for those still toasting the marshmallows of public administration, this post should be a real barn-burner. (For background, previous NC posts on HICPAC: November 9, August 17, August 14, July 20, and July 10.)
Here is a roadmap to the post. I will begin by briefly explaining the HICPAC process, showing the steps by which guidance is developed, where we are in the process, and the documents involved.
Next, I will look at:
(1) HICPAC’s shoddy evaluation of evidence;
(2) HICPAC’s “Evidence Reviews”, unreviewable by the public.
I will then assault HICPAC’s evidence in toto by:
(3) raising statistical issues with every engineering-hating gatekeeper’s favorite tool for minimization, the Randomized Controlled Trial (RCT).
Transitioning to institutional factors:
(4) I will show that HICPAC is conflicted.
Then I will examine two mechanisms for ensuring that guidance as sloppy and degraded as HICPAC’s never sees the light of day:
(5) Performance Reviews under the Federal Advisory Committee Act (FACA), and
(6) The Office for Management and Budget (OMB)’s “Final Information Quality Bulletin for Peer Review.” (These last two items are, so far as I know, original to this post, so after dumping a suitable truckload of salts, bureaucratic knife-fighters and public-spirited lawyers may wish to see if they can be developed further, if only as diversions.)
If you’re already outraged, you can jump directly to the Conclusion, where there are six action items for you.
The HICPAC Process
Here, from CDC itself, is a handy diagram:
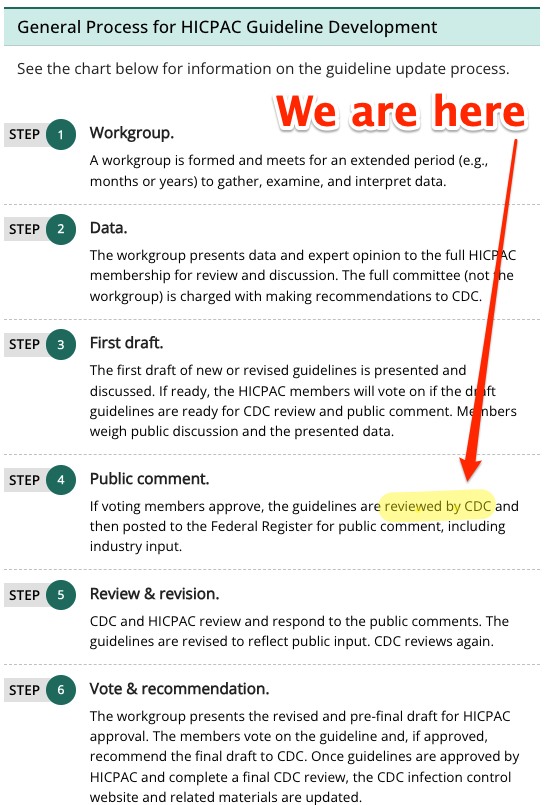
(The same process was used by CDC in developing its guidance for Anthrax.) As you can see, we are in Step 4, “Public Comment, waiting for CDC approval[2]. In prose, again from CDC:
The committee voted on whether the updated (revised) Part 1 draft presented on Day 2 could be sent to CDC for review before posting in the Federal Register. HICPAC met pursuant to the Federal Advisory Committee Act (Public Law 92-463). Part 1 cannot be considered final until posted in the Federal Register for public comment, revised for public comment, and presented and voted on again in 2024.
(Don’t let the stately pace and all the verbiage distract you. This HICPAC guidance development process is as wired up as it can be.)
The CDC describes the documents involved in developing the draft in Morbidity and Mortality Weekly Report:
A CDC guideline is any document issued under agency authority that contains recommendations for clinical practice or public health policy. Recommendations are statements that describe a specific prevention, treatment, or policy action. The scientific evidence underlying these statements is typically obtained through the systematic review of the literature and organized in evidence summaries. These evidence summaries present the causal associations that were critical to the decision-making process used to develop the recommendations.
For the purposes of this post, two documents are relevant. The first is the guidance itself: “2024 Guideline to Prevent Transmission of Pathogens in Healthcare Settings” (in short form, “Guidance”). The second is the systematic evidentiary review: “Healthcare Personnel Use of N95 Respirators or Medical/ Surgical Masks for Protection Against Respiratory Infections: A Systematic Review and MetaAnalysis” (shorter, “Review”).
“Guidance,” through its recommendations, determines policy. HICPAC’s policy proposals are rancid, lethal, and anti-working class. From National Nurses United (NNU):
HICPAC’s draft guidance is aimed at frontline nurses and other health care workers, rather than health care employers, inappropriately shifting responsibility and risk to individual workers to protect corporate profits. The focus of HICPAC’s draft is almost exclusively on personal protective equipment, and it fails to make strong recommendations on other essential measures, such as ventilation and patient screening and isolation.
“HICPAC’s draft is permissive and weak and seeks not just to maintain existing practice — which has been shown to be inadequately protective — but even rolls back the use of some important measures, such as airborne infection isolation rooms,” said NNU President Zenei Triunfo-Cortez, RN. “This draft guidance will only further degrade the already dangerous working conditions of nurses and other health care workers and further contribute to high rates of moral distress, which will only serve to drive more nurses away from the bedside and further deepen the staffing crisis in health care.”
All my previous posts on the HICPAC guidance development process have been focused on the technical foundation of “Guidance,” which is “Review.” In this post, headings (1)-(3) focus on “Review.” Headings (4)-(6) focus on “Guidance,” which incorporates “Review” by reference[3]. More vividly, in (1)-(3) I will dynamite the foundations of the building; in (4)-(6) I will set the entire building on fire. Let’s begin!
(1) HICPAC’s Evidence Is Shoddily Handled
This doesn’t take much. Let’s start with the first set of footnotes in “Review,” 1-5. I have helpfully annotated the screen shot:
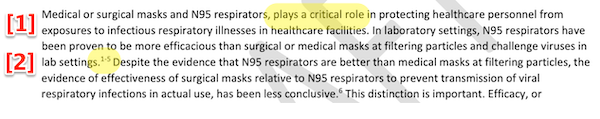
[1] Notice the subject-verb agreement issue, perhaps a sign that too many cooks spoiled the soup of the second paragraph of the introduction. This should not surprise us; we are used to careless copy-editing at CDC.
[2] Notes 1-5 are more interesting, because they direct us to note 2:
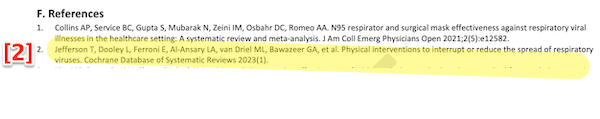
Note 2 refers to the infamous Cochrane study (“Physical interventions to interrupt or reduce the spread of respiratory viruses”). HICPAC writes:
Medical or surgical masks and N95 respirators, plays [sic] a critical role in protecting healthcare personnel from exposures to infectious respiratory illnesses in healthcare facilities. In laboratory settings, N95 respirators have been proven to be more efficacious than surgical or medical masks at filtering particles and challenge viruses in lab settings.
First, the Brownstone Institute-affiliated first author of “Physical interventions” swanned about the media claiming his own study showed that masks were ineffective, for which Cochrane itself had to issue a statement rebuking him:
Many commentators have claimed that a recently-updated Cochrane Review shows that ‘masks don’t work’, which is an inaccurate and misleading interpretation.
It would be accurate to say that the review examined whether interventions to promote mask wearing help to slow the spread of respiratory viruses, and that the results were inconclusive. Given the limitations in the primary evidence, the review is not able to address the question of whether mask-wearing itself reduces people’s risk of contracting or spreading respiratory viruses.
Next, call me crazy, but I don’t think “proven to be more efficacious” (HICPAC, text) means the same as “results were inconclusive” (Cochrane, referring to the study “Physical interventions” mentioned in footnote 2). The “Physical interventions” debacle was a major scandal. Yet not only does HICPAC include “Physical interventions” as a reference, they misrepresent it! I don’t have time to look at the other 91 references, but I don’t think I should have to: One roach in a wedding cake is enough. Obviously, however, somebody should, before it reaches the CDC Director’s desk, let alone the Federal Register. (And do note the interesting possibility that somebody at CDC fixes the subject-verb agreement problem, but leaves the footnote untouched, crossing the boundary between incompetence to maleficence.)
UPDATE In the December 6 Water Cooler, we found a second roach in the wedding cake. Here is the passage from “Review” that contains footnote 6:
Despite the evidence that N95 respirators are better than medical masks at filtering particles, the evidence of effectiveness of surgical masks relative to N95 respirators to prevent transmission of viral respiratory infections in actual use, has been less conclusive.6.
Footnote 6 is the sole external support for this claim by HICPAC. Footnote 6 cites to this study: “Loeb M, Bartholomew A, Hashmi M, Tarhuni W, Hassany M, Youngster I, et al. Medical Masks Versus N95 Respirators for Preventing COVID-19 Among Health Care Workers. Ann Intern Med. 2022 Dec;175(12):1629–38” (“Loeb”). An evaluation of Loeb just came out yesterday, as a preprint: “Failure to protect: COVID infection control policy privileges poor-quality evidence“, by Mark Ungrin, Matthew Oliver, Julia M. Wright, Jonathan Mesiano-Crookston, Malgorzata Gasperowicz, David Fisman, and Corinna Nielson:
The failure to immediately recognize the urgent need to control airborne spread of COVID-19, including use of adequate personal protective equipment for an airborne pathogen, represents a major medical error that cost “an enormous number of lives”. Made in the face of significant scientific evidence and a clear requirement to adhere to a precautionary approach, it has still not been fully remedied. To understand the substantial, ongoing gap between science and policy, we carried out an in-depth investigation of an illustrative publication [Loeb] authored by prominent authorities in the fields of Public Health and Infection Prevention and Control, describing a trial of medical masks and N95 respirators for the prevention of COVID-19. Although it was portrayed as among the highest quality evidence available within the Evidence-Based Medicine decision- making paradigm, we found this work to be deeply flawed to the extent that it does not meet basic standards of scientific rigour. Extensive prior work in the respiratory protection field – sufficiently well-established to be incorporated into both national standards and specific recommendations made to address infection control failures in SARS – was ignored. Randomization was compromised, with a statistically significant correlation between female sex and allocation to the higher- risk arm of the trial. Significant conflicts of interest in favour of the reported finding that medical masks are noninferior to N95 respirators in preventing COVID-19 transmission were not disclosed. Prespecified analyses were omitted, and the finding of noninferiority is entirely a product of inappropriate alterations to the trial that were not prospectively registered. Despite numerous flaws biasing the outcome towards a finding of noninferiority, re-analysis using the prespecified approach and noninferiority criterion unambiguously reverses the reported outcome of the trial.
So the intern cleaning up the systematic review is going to have even more work, poor devil.
(2) HICPAC’s “Evidence Reviews” were Unreviewable by the Public
In my previous post on “Review,” I had only a PowerPoint presentation to work with (CDC having violated FACA by not making drafts available). I criticized the PowerPoint for failing, as claimed, to meet the PRISMA protocol, and for not disclosing Division of Healthcare Quality Promotion (DHQP) scales used to assess the validity of the studies. Those defects in “Review” are remedied in the complete draft.
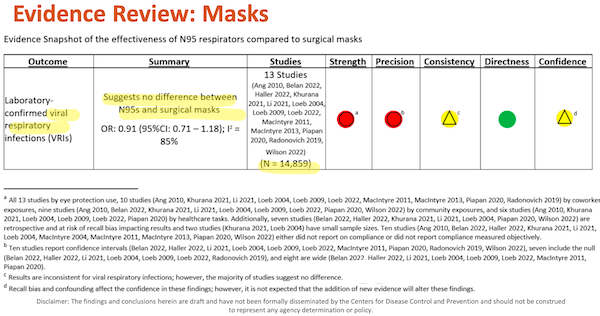
However, the salient features of the “Evidence Reviews” in “Review” are contained in tables, called “Evidence Snapshots”. Here we have the technical foundation of “Guidance,” since these tables purport to show that N95s and “Baggy Blues” are equivalent in hospital and managed care settings, a finding that permits HICPAC’s recommendations. Here are the relevant tables in the PowerPoint presentation in August (highlighted by me):
And:
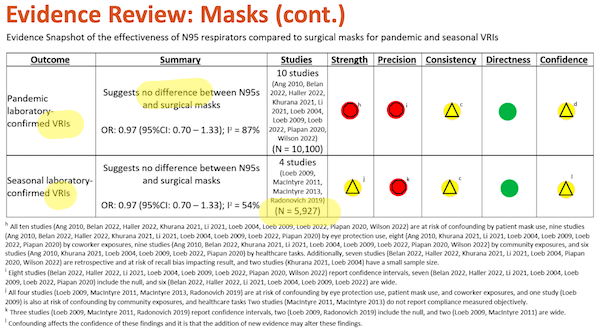
In November’s draft, you can see that August’s two tables are consolidated into one:
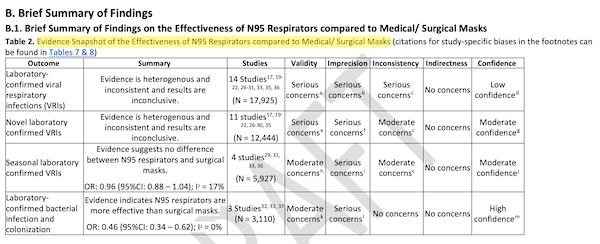
Moreover, if you compare the Outcomes, Summaries, and Studies columns in August with those in November, they all differ.
This matters, because in reviewing the August PowerPoint, I disaggregated both highlighted tables above, and created my own table. I turned every study footnoted in the Studies column into a row, ranked each individual row by study strength, precision, confounders, and other negative factors — all from CDC’s data! Then I sorted my table. The “best” studies ranked highest, and lo and behold! They were all pro-respirator (see NC here).
In other words, HICPAC jiggered its own data. Putting matters more politely, as I did in the original post:
3. I’d very much like to believe that when I disaggregate [the tables in] Slides 31 and 32, and pro-respirator, anti-Baggy Blue studies — to everyone’s utter surprise! — float to the top, that I have committed an error, and that HICPAC and CDC are on the up-and-up, having learned something from CDC’s initial debacle on mask policy, and its losing tooth-and-nail battle against the science and engineering of airborne transmission…. CDC has form. A hermeneutic of suspicion is fully justified.
National Nurses United comments on the amount of time CDC made available for a public review:
Despite the critical importance of this infection control guidance, the CDC/HICPAC is only accepting written public comment on the draft until 11:59 p.m. on Monday, Nov. 6, giving the public a mere five days to review the 24-page document and 162 pages of supporting documentation and provide feedback.
The tables in the August PowerPoint version of “Review” were the technical foundation of “Guidance”; that is why HICPAC’s working group requested them. And yet, in November’s version of “Review,” the technical foundation of “Guidance” has been completely altered. The August tables were already a Gish Gallop. Does HICPAC really expect the public to run a second Gish Gallop, in only five days?
(3) HICPAC’s Randomized Controlled Trials (RCTs) Are Statistically Invalid
Yaneer Bar-Yam, Jonathan M. Samet, Alexander F. Siegenfeld, Nassim N. Taleb published “Quantitative errors in the Cochrane review on ‘Physical interventions to interrupt or reduce the spread of respiratory viruses'” in October of this year. However, the implications of their article go far beyond their demolition job of Cochrane (reviewed by our own KLG here). From the Abstract:
N95 respirators, and other forms of respiratory protection, have proven efficacy in reducing the risk of infection across various environments. Even though multiple studies confirm their protective effect when adopted in healthcare and public settings for infection prevention, studies on their adoption over the last several decades in both clinical trials and observational studies have not provided as clear an understanding. Here we show that the standard analytical equations used in the analysis of these studies do not accurately represent the random variables impacting study results. By correcting these equations, it is demonstrated that conclusions drawn from these studies are heavily biased and uncertain, providing little useful information. Despite these limitations, we show that when outcome measures are properly analyzed, existing results consistently point to the benefit of N95 respirators over medical masks, and masking over its absence. Correcting errors in widely reported meta-analyses also yields statistically significant estimates. These findings have important implications for study design and using existing evidence for infection control policy guidelines.
In short form, every RCT cited in “Review” is invalid until proven otherwise. More work for the hapless intern straightening out the “evidence snapshots”!
(4) HICPAC’s Membership Is Conflicted
From the technical foundations of “Guidance” in “Review,” we now turn to larger, institutional factors. Again from CDC, “Standards Required for the Development of CDC Evidence-Based Guidelines“:
The Federal Advisory Committee Act (FACA) provides the framework for consulting with experts outside the federal government to provide advice on appropriate recommendations (16). FACA delineates how federal advisory committees [like HICPAC] should be operated and managed… Users of CDC guidelines and recommendations need to know that financial, professional, or personal interests have not influenced the development of recommendations. A competing interest exists when professional judgment or actions concerning a primary interest, such as patients’ or the public’s welfare or the validity of research, might be improperly influenced by a secondary interest, such as financial gain, professional advancement, or personal relationships.
Every HICPAC member is affiliated with a hospital, and all these hospitals have already adopted masking policies as weak and lethal as “Guidance” proposes, as I show here. The conflicts are three-fold: Trivially, HICPAC members are conflicted because the cost of respirators will appear as a budget line-item for the infection control departments to which many of them belong (“professional advancement”). From NNU in MedPage Today:
After nearly 4 years of living with the COVID pandemic, we have all learned hard lessons about PPE and how healthcare employers often focus on the bottom line rather than protecting healthcare workers and patients.
Second, HICPAC members would incur reputational damage for adopting, as CDC guidance, a masking policy more protective of patients and workers than the policies they have already adopted for their own institutions, whether formally, or complicitly (“personal relationships”). People might ask questions!
Third (“financial gain”), the avoidance of liability:
As an industrial hygienist, [Peg Seminario, a retired safety and health director for the AFL-CIO,] was extremely critical that there were no experts in respiratory protection on the committee nor did it include engineers who developed ventilation guidelines. She believes that the some oppose respirators “because once you are into recommending respiratory protection, with that comes a full respiratory protection program from OSHA,” with penalties for violations.
An epidemiologist and consultant, Michael Olesen, echoed this, citing “pressure to remove liability from hospitals.” He added, “I take a very clear position that we should be having respiratory protection mandates in all healthcare settings right now.”
And on the Twitter:
On HICPAC/CDC wanting to kneecap infection control: the lower the standard of care, the lower the liability, the lower the insurance premiums. Healthcare is defending lawsuits before they happen by setting fire to infection control standards and PPE requirements
— Justin Lee (@DailyJLee) August 22, 2023
One hates to be cynical. But this is the CDC. In any case, HICPAC is clearly riddled with “secondary interests,” and the work product of such an entity should not reach the CDC Director’s desk for approval.
UPDATE On liability, we found this, also in the December 6 Water Cooler: “Negligence Cases Against Hospitals for Negligent Transmission of Coronavirus“, from Arnold and Smith Personal Injury Lawyers in North Carolina:
Persons infected in a hospital with COVID-19 may pursue claims against the facility for the following potential breaches of the duty to exercise reasonable care:
- Failure to adequately train staff on how to properly deal with patients exhibiting virus symptoms;
- Failure to test employees and patients for the virus;
- Failure to screen employees and patients for symptoms;
- Failure to enact reasonable safety protocols such as mandating the use of protective clothing and requiring social distancing measures to protect patients;
- Failure to quarantine patients exhibiting COVID-19 symptoms;
- Failure to screen hospital guests for symptoms;
- Failure to enact disinfectant and social distancing guidelines for employees;
- Failure to close facilities to guests, to protect patients.
If a hospital failed to take reasonable steps to protect patients from exposure to COVID-19, a person injured by the facility’s negligence may be entitled to bring a claim against the hospital. The professionals at Arnold & Smith, PLLC can assist hospital patients or guests who believe they contracted COVID-19 at a hospital.
Consultations are said to be free. Big hospitals like Mass General have been driving HICPAC toward guidance that lowers patient and staff protections MR SUBLIMINAL “Baggy Blues 4EVA!” throughout the HICPAC process, as I show here. They all have legal departments. It’s hard to believe they haven’t been thinking about liability from the beginning of the pandemic (or speculating freely, discovery might show they have already had strategies prepared, having done the math after, say, MERS or Ebola, and are only now using HICPAC to operationalize them. Sadly, Mass General had no Cuomo to protect them).
(5) HICPAC’s Treatment of Public Comments Is So Belittling As To Trigger a Performance Review Under FACA
Let’s begin by establishing that public comments are, in fact, valuable. In Academic Medicine, “Why Public Comments Matter: The Case of the National Institutes of Health Policy on Single Institutional Review Board Review of Multicenter Studies,” from the Abstract:
In this case study, public comments were effective in shaping policy as the NIH modified provisions or planned supplemental guidance in response to comments.
And from the Center for Medicare and Medicaid Services, “Public Comments“:
CMS encourages public comments and the submission of additional medical, technical, and scientific evidence, and must respond to these comments in our final determination as required by law. Public participation increases the quality of agency decision making.
However, HICPAC members, by their actions, disagree. Here is a live tweet storm that shows some of their belittling behaviors. Chatting on cellphones:
Making live edits:
Replacing public commenter’s faces with timers on Zoom (priorities!):
(No doubt a review of the video would find more such behaviors.)
HICPAC is governed by Federal Advisory Committee Act (FACA), which is administered by the General Services Adminitration (GSA). The GSA has established “Performance Guidelines“:
[GSA’s FACA] Administrator shall prescribe administrative guidelines and management controls applicable to advisory committees, and, to the maximum extent feasible, provide advice, assistance, and guidance to advisory committees to improve their performance. In carrying out his functions under this subsection, the Administrator shall consider the recommendations of each agency head with respect to means of improving the performance of advisory committees whose duties are related to such agency.
(Bold in the original.) Put aside the issue of only five days for public comment on “Guidance” when it had an entirely new technical foundation in November’s “Review.” Can anyone really believe that HICPAC members diddling with their cellphones during public comment — not to mention the meeting chair who permitted this discourtesy — does not require intervention by a GSA Administrator committed to improving HICPAC’s “performance” “to the maximum extent feasible“? And clearly, deliverables produced by such a Committee, unserious with respect to public comment from, among others, experts in the fields of aerosols, ventilation, and industry who don’t happen to work for hospitals, should not reach the CDC Director’s desk for approval.
(6) As a “Highly Influential Scientific Assessment,” HICPAC’s Guidance Must Be Vetted Under OMB’s “Final Information Quality Bulletin for Peer Review”
The NNU explains why “Guidance” (and its technical foundation, “Review”) are influential:
The draft Isolation Precautions Guideline, which was only released to the public yesterday, Nov. 2, is an extremely influential document that directs infection control practices for health care facilities in the United States. This guidance, which has not been updated in 16 years, will be referenced by U.S. employers and government agencies across the country and also by health agencies around the world.
As it turns out, there’s a review process for “influential” documents. From the Bureau of Reclamation (USBR) in 2023:
The Office of Management and Budget (OMB) directive, Final Information Quality Bulletin for Peer Review, dated December 16, 2004 (263 KB PDF), requires that there be a “systematic process of peer review planning” and public access to a list of information products for that will be peer reviewed as either influential scientific information or highly influential scientific assessments.
The USBR provides a handy table of projects that fall under the aegis of “Highly Influential Scientific Assessments.” One of them is the “Anderson Ranch Water Quality Model.” Surely we can agree that if a water modeling study of a river in Idaho falls under the aegis of OMB’s “Final Information Quality Bulletin,” then “Guidance” (and “Review”), which will affect the health and the lives of millions of hospital patients and workers, should do so as well? OMB agrees. From “Final Information Quality Bulletin for Peer Review“:
The term “influential scientific information” means scientific information the agency reasonably can determine will have or does have a clear and substantial impact on important public policies or private sector decisions.
Here are OMB’s requirements for how “influential scientific information” should be peer-reviewed:
Regardless of the peer review mechanism chosen, agencies should strive to ensure that their peer review practices are characterized by both scientific integrity and process integrity. “Scientific integrity,” in the context of peer review, refers to such issues as “expertise and balance of the panel members; the identification of the scientific issues and clarity of the charge to the panel; the quality, focus and depth of the discussion of the issues by the panel; the rationale and supportability of the panel’s findings; and the accuracy and clarity of the panel report.” “Process integrity” includes such issues as “transparency and openness, avoidance of real or perceived conflicts of interest, a workable process for public comment and involvement,” and adherence to defined procedures.
A proper peer review of HICPAC’s guidance would find, as we have shown above, conflicts of interest. Such a review would also find a completely unworkable “process for public comment” (indeed, a process sabotaged by the belittling and exlusionary actions of HICPAC members themselves). In addition, if the peer reviewers included, as they should, aerosols, ventilation, and industrye experts, they would surely find that “expertise and balance of the panel members” were lacking. So “Guidance” is marked neither by “scientific” nor “process” “integrity.” Unsurprisingly, for those who have been following this saga.
Note further this requirement from OMB:
Draft influential scientific information presented at scientific meetings or shared confidentially with colleagues for scientific input prior to peer review shall include the disclaimer: “THE FINDINGS AND CONCLUSIONS IN THIS REPORT (PRESENTATION) HAVE NOT BEEN FORMALLY DISSEMINATED BY [THE AGENCY] AND SHOULD NOT BE CONSTRUED TO REPRESENT ANY AGENCY DETERMINATION OR POLICY.”
Here is HICPAC’s footer for “Review”:
Disclaimer: The findings and conclusions herein are draft and have not been formally disseminated by the Centers for Disease Control and Prevention and should not be construed to represent any agency determination or policy.
Not in all caps, but clearly OMB’s verbiage. I would urge that this virtual identity in wording shows that HICPAC is fully aware of its obligations under OMB’s “Final Information Quality Bulletin,” but has chosen to go ahead with a conflicted and unbalanced MR SUBLIMANAL Not that way. Or maybe…. committee regardless. I don’t know at what point OMB should intervene — Before the Federal Register? After? — but intervene they should, because a draft so lacking in integrity should not be presented to the CDC Director for approval.
Conclusion
Frankly, the whole HICPAC process is so deficient as to warrant testing for loss of executive function due to Covid infection by its members MR SUBLIMINAL Lawyers reading this, you know you want to file that lawsuit. Nevertheless, there are things that each one of us can do.
First, watch the skies for the opening of the comment period in the Congressional Record after CDC Director “Maskless Mandy,” by some opaque, oracular process, approves “Guidance.”
Second, call the Inspector General of Health and Human Services with additional HICPAC defects (i.e., others not identified here). This post at NC explains how and why, and presents a suggested script.
Third, sign any of the various petitions floating around. This one:
Urge CDC Director Mandy Cohen to Reject HICPAC’s Draft and Protect Health Care Workers and Patients from Infectious Diseases! https://t.co/GVsBn44mIw
— Adrian (@SillyPutty78) December 3, 2023
Or this one:
Another round to push back against @CDCDirector @CDCgov as the #HICPAC fails to protect healthcare workers and patients. If you have a scientific background or work in medicine or healthcare or public health please sign at this link! #medtwitter due Friday, dec 8th!… pic.twitter.com/7TaxkUlHg2
— Andrew W a n g, PhD, MPH, CPH (@AWangMPH) December 2, 2023
I’m sure there are others; readers may add in comments.
Fourth, call or write your Congress Critter:
<if you can't or don't want to call your 🇺🇲 congressional reps, & you'd rather email them>
👇https://t.co/GZryW6EMg7https://t.co/uiVMbpck6e— Moriah (Galores Flying Circus) (@GaloresCircus) November 25, 2023
Fifth, write a letter to the editor of your local newspaper[4]. (I’m a big fan of LTEs. They get read in your elected’s office, and in the executive suites of your town. And I still remember getting a thumb’s up from a passing car because of a letter I wrote to the Bangor Daily News over the landfill.)
Sixth, however, it may well be that for airborne protection, and clean air generally, some organization on the order of ACT UP — can anybody come up with an expansion for the acronyn AIRBORNE? Great vibe — may be needed in the long haul. From Teen Vogue:
ACT UP is an activist movement born out of the crisis of the HIV/AIDS epidemic. In the face of deep-seated homophobia and indifferent federal and state governments, its members have relied on civil disobedience and protests to win sympathy from the public and goad recalcitrant officials into action. ACT UP has gone after pharmaceutical companies, championed harm-reduction policies, and fought to repeal discriminatory policies and ordinances that target women and the LGBTQ+ community.
Established on March 12, 1987 as a political action group, ACT UP’s focus would not be on raising funds or providing care, but using direct action and civil disobedience to highlight the failures of society and the political system to care for people with HIV/AIDS.
What lessons can we learn from ACT UP? Says Schulman, “The most important takeaway is that ACT UP was not a consensus-based movement. By that I mean people did not have to agree in order to do things. It had a bottom line, and every movement has to have a bottom line, and theirs was a one-line statement of unity: ‘direct action to end the AIDS crisis.'”
(There’s also an uncomfortable parallel between the “ID” (Immune Deficiency) in AIDS, and immune dysregulation from Covid, for which the ultimate non-pharmaceutical information is clean air, especially indoor air.) So do give consideration to supporting such an organization, should it arise.
A hospital should not be a place where you get sicker:
An actual convo I just had:
Family member: I had a bad reaction to my anesthesia from surgery last week
Me: Oh no what happened
Fam: I’ve been fatigued, feverish & congested the past 4 days
Me: That sounds like a virus
Fam: Not possible, the only place I’ve been is the hospital pic.twitter.com/xTuQb9WY0f— 🐀 (@Guiness_Pig) December 3, 2023
NOTES
[1] Sources treat “guidance” and “guideline” as synonyms. I prefer “guidance.” Public administration mavens correct as needed.
[2] CDC is noticeably opaque on how it — presumably in the person of its Director — approves the guidance, and then forwards the guidance onward to the Federal Register for another round of comments. Perhaps some kind reader will leave a link in comments, or throw something over the transom. (You can find my address at the bottom of Water Cooler just before the plant of the day.)
[3] From “Guidance“:
In order to provide context to the update of the 2007 Guideline’s Transmission-Based Precaution categories, the authors requested three systematic reviews from DHQP that answered questions on the performance of several PPE items. These systematic reviews, which were not conducted to support the development of specific recommendations, answered the following key questions: 1. For healthcare personnel caring for patients with respiratory infections, what is the effectiveness of N95 respirators compared to medical/surgical masks in preventing symptomatic illness or laboratory649 confirmed infection? [cite webpage].
I just love “[cite webpage].” As you can see, CDC is, as it were, pulling the ladder up after itself by concealing the technical basis for its recommendations (and how that basis shifted over time).
[4] I don’t think, in this case, “the media” is entirely a lost cause. Coverage of HICPAC has been more frequent and more balanced than I would have expected: CNN, Discovery, Drugs.com (!), Forbes, GB News, Infection Control Today, KION, MedPage Today, and US News. I’m sure there are others, so I wouldn’t write the media off, at least in this case.


[taps mike.]
What is HICPAC? (Please explain/define acronyms like this at the beginning of articles.)
Hospital Infection Prevention and Control Advisory Committee of the CDC. IPC is the general acronym used by hospitals for infection control.
Dang. Thought I got ’em all. Fixed.
Great headline, will screenshot well for sharing!
“A hospital should not be a place where you get sicker”
Yep.
I can’t help but wonder where physicians are in this fight. Have they been so demoralized by the neoliberal infestation of healthcare (and our general mindset) they have no fight left?
Thanks for the article, it’s an important topic. As an old person with health conditions that will likely put me in a hospital again, the danger is real, and personal.
Healthcare settings are the places where I have never relaxed masking — I mean, that’s where sick people congregate, right?
Here in New York recently I’ve had my great old Primary Care refer me to several young “entrepreneurs” who are all business: in medicine to make a buck. Neoliberal, retired or about to are the three categories of MDs these days.
Thank you, Lambert.
> A hospital should not be a place where you get sicker
From the standpoint of a healthcare provision system that strives to maximize revenue and profits, nosocomial infections might be features rather than bugs.
In addition to reducing short-term operating costs, inadequate infection control practices probably increase top-line revenue.
—-
snark off, I have a very bad feeling about all this. Some proportion of the population is already delaying care due to cost. Turning healthcare visits into spreading events is going to further deter people from seeking non-emergency care.
Also deter people from pursuing careers in healthcare.
This was my initial thought as well. I wouldn’t want any of my loved ones pursuing a career in this field.
> Turning healthcare visits into spreading events is going to further deter people from seeking non-emergency care
Surely many immuno-compromised people are delaying care, which is unfortunate, since often they are the most in need of it, and must invest the most energy and time getting it (see under Stochastic Eugenicism).
But then we have the financial barriers to seeking care, which affects everybody.
I worry about people turning to folk remedies and quack nostrums (the whole “immunity debt” thing, ditto (God-given)) “natural immunity,” and the idea that immunity is like a muscle that becomes stronger as it’s challenged, plays into this mentality).
The U.S. surge is worsening faster than anticipated…
https://twitter.com/michael_hoerger/status/1731794087655653416
It is all quite grim. What happens as medical personnel experience repeated infection much more frequently than gen pop? Quality of care will just dissolve.
I can’t shake the feeling that Stephen King’s The Mist has rolled across this country. By all means mask up and protect yourself, but what’s the point if everyone around you falls apart like Sally from Nightmare Before Christmas?
> What happens as medical personnel experience repeated infection much more frequently than gen pop?
I imagine those who really know the score will have left an environment where they can no longer protect themselves from breathing a Level Three Biohazard in shared air, leaving — worst case scenario — delusional Smile Nazis in charge. The same in the schools. And air traffic control towers. Etc.
I have only anecdotal evidence of this, of course. Surveys will be taken and studies done only when the rot is very far advanced. But readers are welcome to share anecdotes!
Didn’t NC do some coverage of the US credits and incentives for improving air quality, and how much of that money hasn’t been used? And how the Healthcare settings that have quietly amped up already very good air circulation to be tremendously good are not saying a mumbling word about what they’ve done and how much monitoring they’re doing? Or do I know that from other avenues.
There’s no way to know, of course. Unless you’re on the board or working an accounting, purchasing, of facilities management at a particular healthcare facility.
But my point is, all hail Lambert for exhaustive coverage of this debacle.
This all sounds like a standard bureaucratic tactic. If you select the people on a committee or even a majority, they will deliver up the recommendations that you want. You saw this with the people that were picked to investigate January 6th and you will note that it was hinted at in their name – the House ‘Select Committee’. Here it might be more of a case of picking people that ‘follow the narrative’ and who know that by disagreeing with the narrative, that it will end their lucrative, comfortable PMC lifestyle. And when HICPACS delivers up the report that the CDC want, the CDC can say that it was an independent committee that put these recommendations together, not them, so of course they will be obliged to follow those recommendations.
> This all sounds like a standard bureaucratic tactic.
Of course. HICPAC is wired to advances the interests of the hospital monopoly, more precisely “infection control” departments [pause for bitter laughter] within those hospitals, as I have shown here. As ever, the lunch is naked.
The degree to which past best practices, even statutorily required practices, have been abandoned in the background with the pandemic being the big reveal is starting to become generally apparent.
It’s much like the rot in UK administrative practice for construction safety that led to the Grenfell debacle. The UK essentially invented fire safety/life safety codes during the Blitz, a fascinating story of volunteer engineers monitoring and manipulating ingress and egress from the Tube/bomb shelters before and after air raids.
Much as the CDC set up, in the pre-neoliberal era, the gold standard for public health, UK public works administrators set up building safety only to have all the public good embedded in the system grifted and looted away over several generations like termites eating a shotgun shack in New Orleans until one day someone slams the door and the whole thing falls down.
Any hospital following HICPAC guidance is going to face enormous liability, there’s no way a “Professional” infection control specialist can pretend they don’t know about the problems with HICPAC given all the publicity.
As I understand it, the whole point is that CDC Guidance is a Get Out Of Jail Fee card for Private Equity, I mean hospitals.
You sue and they say we were following guidelines. IANAL, can you sue the Federal Government when the hospital/PE wins?
If not, the electoral change is the answer, but in Pay to Play money always wins, so voting for a “reform” candidate becomes like voting for Zelensky because he ran on peace with Russia.
The last three years have ensured “guidance” is permanently on my list of words when I read or hear it, instantly causes my suspicion/b.s. meter to peg the needle off the dial. Whatever the “guidance” is, you should probably be doing the opposite. (Mask when they say not to)
It’s as though the CDC’s policy is “Questions are a burden to others; answers are a prison for oneself”. If that quote seems familiar, you’ve probably have seen or are a fan of the 1967 TV series The Prisoner.
Thank you for your efforts on this, Lambert. NC is one of the only resources remaining for people who haven’t fallen for establishment propaganda but who want to keep up with new developments regarding covid.
I’m not surprised that HICPAC is composed of sociopaths, what does surprise is that they don’t seem to have any sense of self preservation.
These are senior people in their 40’s and up, do none of them expect to need cancer surgery or a hip replacement?
Some of them may even care about a spouse or a child, as unlikely as that may seem.
THANK YOU for staying on top of all of this for us.
“A hospital should not be a place where you get sicker”
A century ago, a trip to a hospital was one of the deadliest activities – before sanitation, the germ-theory of disease, and antibiotics. Modern medicine as we know it today is almost miraculously safe! And instead of keeping it that way, our rulers seem to be moving us backwards.
[lambert blushes modestly]
About a month ago my father was admitted from nursing home to a hospital in NW Wisconsin for a UTI. Docs noticed a cough a day or two later, had him tested for covid with results returned a day later as positive.
I later learned that each of the other six patients on his side of the hospital wing tested positive too, however, multiple patients at the nursing home from which he had come were ill with covid as well.
These are the only two places where he could have aquired the covid infection, and both a healthcare settings.
I’m not sure why I’m surprised, but the depravity HICPAC members display in the public comments hearing is still shocking. Petitions signed. Thanks.