By Lambert Strether of Corrente
Once again I must put on my Mr. Pandemic™ hat, following up on the previous post, “Will Human-to-Human Bird Flu (H5N1) Be the Long-Awaited “Disease X?”,” and noting that — touch wood — Beveridge’s Law still applies. Displaying the sunny temperament for which I am so well-known, let me begin with some good news: We can test wastewater for H5N1. From the following preprint, “Detection of hemagglutinin H5 influenza A virus sequence in municipal wastewater solids at wastewater treatment plants with increases in influenza A in spring, 2024” (sadly, horrid Alphabet’s Verily, and not our old favorites, Biobot). From the Abstract:
Prospective influenza A (IAV) RNA monitoring at 190 wastewater treatment plants across the US identified increases in IAV RNA concentrations at 59 plants in spring 2024, after the typical seasonal influenza period, coincident with the identification of highly pathogenic avian influenza (subtype H5N1) circulating in dairy cattle in the US. We developed and validated a hydrolysis-probe RT-PCR assay for quantification of the H5 hemagglutinin gene. We applied it retrospectively to samples from three plants where springtime increases were identified. The H5 marker was detected at all three plants coinciding with the increases. Plants were located in a state with confirmed outbreaks of highly pathogenic avian influenza, H5N1 clade 2.3.4.4b, in dairy cattle. Concentrations of the H5 gene approached overall influenza A virus gene concentrations, suggesting a large fraction of IAV inputs were H5 subtypes. At two of the wastewater plants, industrial discharges containing animal waste, including milk byproducts, were permitted to discharge into sewers. Our findings demonstrate wastewater monitoring can detect animal-associated influenza contributions, and highlight the need to consider industrial and agricultural inputs into wastewater. This work illustrates the value of wastewater monitoring for comprehensive influenza surveillance for diseases with zoonotic potential across human and animal populations.
It’s actually good news that finally we can have some sense of how much H5N1 there is out there, but at the same time, human-excreted and Concentrated Animal Feeding Operation (CAFO)-derived H5N1 both go into the same waste stream, as the authors themselves remark in the Discussion, so we can’t get a good reading on how many people have H5N1 from this data alone, i.e., whether there’s a pandemic or not (though I imagine some work could be done with location, i.e., non-CAFO sewersheds).[1]
ln the remainder of this post, I will first look what we now know about H5N1 transmission and mutation, and then at protecting the food supply from H5N1 (with an aside on characterizing H5N1 as a food supply problem; basically, at what is known today as opposed to what was known when last I posted. (Readers will, of course, supply any lacunae; it’s a fast-moving story). Finally, I consider the posssibility of an H5N1 pandemic in the light of the precautionary principle we so conspicuosly failed to apply in the current, ongoing pandemic, SARS-CoV-2.
H5N1 Transmission and Mutation
Here are all the examples of transmission between mammals (including humans) that I could find. (Here is a case of transmission from birds to dolphins).
Cattle to cattle and cats. From the CDC, “Highly Pathogenic Avian Influenza A(H5N1) Clade 2.3.4.4b Virus Infection in Domestic Dairy Cattle and Cats, United States, 2024.” This is, I believe, the epicenter of detection, though not necessarily “Cow Zero” as it were:
In February 2024, veterinarians were alerted to a syndrome occurring in lactating dairy cattle in the panhandle region of northern Texas. Nonspecific illness accompanied by reduced feed intake and rumination and an abrupt drop in milk production developed in affected animals. The milk from most affected cows had a thickened, creamy yellow appearance similar to colostrum. On affected farms, incidence appeared to peak 4–6 days after the first animals were affected and then tapered off within 10–14 days; afterward, most animals were slowly returned to regular milking. Clinical signs were commonly reported in multiparous cows during middle to late lactation; ≈10%–15% illness and minimal death of cattle were observed on affected farms….
In early March 2024, similar clinical cases were reported in dairy cattle in southwestern Kansas and northeastern New Mexico; deaths of wild birds and domestic cats were also observed within affected sites in the Texas panhandle. In >1 dairy farms in Texas, deaths occurred in domestic cats fed raw colostrum and milk from sick cows that were in the hospital parlor. Antemortem clinical signs in affected cats were depressed mental state, stiff body movements, ataxia, blindness, circling, and copious oculonasal discharge. Neurologic exams of affected cats revealed the absence of menace reflexes and pupillary light responses with a weak blink response.
On March 21, 2024, milk, serum, and fresh and fixed tissue samples from cattle located in affected dairies in Texas and 2 deceased cats from an affected Texas dairy farm were received at the Iowa State University Veterinary Diagnostic Laboratory (ISUVDL; Ames, IA, USA). The next day, similar sets of samples were received from cattle located in affected dairies in Kansas. Milk and tissue samples from cattle and tissue samples from the cats tested positive for influenza A virus (IAV) by screening PCR, which was confirmed and characterized as [Highly Pathogenic Avian Influenza (HPAI)] H5N1 virus by the US Department of Agriculture National Veterinary Services Laboratory. Detection led to an initial press release by the US Department of Agriculture Animal and Plant Health Inspection Service [APHIS] on March 25, 2024….
Cattle to humans. From Stat, “What we’re starting to learn about H5N1 in cows, and the risk to people,” a vivid description of a “milking parlor” (there’s plenty more):
Milking parlors are typically enclosed buildings outfitted with individual stalls arranged in a ring or in rows where dairy cows are led two to three times each day to drain their udders of milk. In a milking operation, the stimulus to secrete milk comes not from the sight or touch of a calf but is usually provided by a farm worker. That person also cleans the animal’s teats with a damp cloth and then dips them into a disinfectant solution to protect them from infectious bacteria present on a farm. The teats are then attached to the milking unit, also called a claw, which consists of a cluster of four rubber or silicon-based liners that fit snugly around each teat. The milking lasts about six to nine minutes per animal, and then each cow receives another disinfectant treatment before it’s ushered out and another animal is brought in.
The problem is that the milking equipment that comes into contact with the cow’s udders is typically not sanitized between individual animals, said Nigel Cook, a professor in Food Animal Production Medicine at the University of Wisconsin-Madison and long-time dairy cow health researcher. Rather, sanitization steps happen only two or three times a day.
“Contamination of the milking unit with milk residue cross-contaminating to the next cow would be a risk — as it would with any mastitis pathogen,” Cook told STAT via email.
Liners also have to be regularly replaced, as wear and tear and chemical exposure make them lose their elasticity, becoming rough and split. When that happens, the liners are more difficult to disinfect and can act as a reservoir for infection.
Liners, dip cups, washrags, and milkers’ gloved hands are all possible means of spreading the virus from one animal to the next. Washrags used on different animals are often laundered together before repeat use, but some dairies don’t use hot water, and researchers have found genetic traces of H5N1 on both used and clean rags using PCR testing. More work is needed to figure out which vectors are playing the biggest role, scientists told STAT.
Only one human infection — a Texas dairy farm worker who developed conjunctivitis — has been reported, but anecdotal reports abound of other farm workers with conjunctivitis and mild respiratory symptoms. Scientists at the Centers for Disease Control and Prevention are working to figure out where the biggest risks to these workers lie, Sonja Olsen, associate director for preparedness and response in CDC’s influenza division, said during the ASTHO symposium. Is it exposure to cows? Contact with milk? Are there specific activities on farms or in slaughterhouses that put people at elevated risk of contracting H5N1?
I assume “exposure to cows” means transmission “through the air,” and indeed that’s mentioned as possibility, which is refreshing. (It’s entirely possible for both fomite transmission through the “milking unit” and airborne transmission to occur.)
Wild animals generally. Here is a handy map of all the animals in which H5N1 is to be found, and where they occur’ some birds, lots of mammals (plus the oppossum, a marsupial). From APHIS:
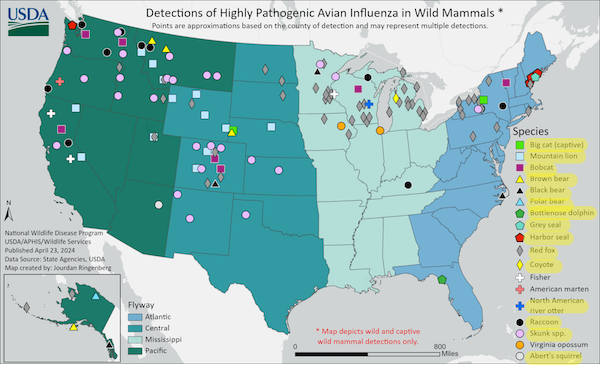
(Given how deer infest so many suburban neighborhoods, it would be bad if they were carriers, but apparently the likelihood is low.)
Now, I don’t raise all these examples because they reach pandemic status, alone or together. I raise them because the more H5N1 is “out there,” the more likely it is that a mutation will occur that does reach pandemic status. From Time, “Why Experts Are Worried About Bird Flu in Cows“:
[Health experts are] watching how the virus moves from species to species and what genetic changes it picks up as it makes these jumps. Bird flu strains aren’t generally adept at infecting other species, including mammals. But the most recent case of bird flu in a person was also the first time the virus has been found in cows.
The fact that it’s now infecting cows—animals that people come in closer contact with than other mammals that have harbored H5N1, like foxes—means the viruses could potentially be mutating in ways that could spread and cause disease in significantly more people.
[Andrew Bowman, associate professor of veterinary preventive medicine at Ohio State University] says that the FDA’s report is concerning because it suggests that this particular strain of H5N1 is continuing to be transmitted among cows. ‘This is a spillover into a mammalian host that seems to be maintaining [the infection],’ he says. ‘In previous spillovers into mammals, it seemed to be for the most part individual events that were isolated and didn’t continue to spread in those species. This is different.’
“Every time another animal or human is infected, it’s another throw at the genetic roulette table in terms of whether the virus could become one that transmits from human to human, which is what is required for a pandemic,” says Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota. “If you throw enough times, you may end up with an outcome that you don’t want.”
(Osterholm’s “throw at the genetic roulette table” is Taleb’s “risk of ruin,” which we’ll get to when we discuss the Precationary Principle). In the meantime, at least one mutation has occurred. From Alexander Tin, “HHS press briefing on avian influenza”:
[MIKE WATSON, APHIS] Also on April 16th, USDA APHIS microbiologists identified a shift in the H5N1 sample, this is one sample from a cow in Kansas, that could indicate that the virus was mutating for adaptation to mammals.
However, CDC conducted further analysis of the specimen sequence and their assessment is low risk over all, of this one sample that has that change.
Oh. (CDC’s “low risk” is clearly not Taleb’s “risk of ruin.”)
Protecting the Food Supply from H5N1
Milk. From Stat, “H5N1 bird flu virus particles found in pasteurized milk but FDA says commercial milk supply appears safe“:
Testing conducted by the Food and Drug Administration on pasteurized commercially purchased milk has found genetic evidence of the H5N1 bird flu virus, the agency confirmed Tuesday. But the testing, done by polymerase chain reaction, or PCR, cannot distinguish between live virus or fragments of viruses that could have been killed by the pasteurization process.
The agency said it has been trying to see if it could grow virus from milk found to contain evidence of H5N1, which is the gold standard test to see if there is viable virus in a product. The lengthy statement the agency released does not explicitly say FDA laboratories were unable to find live virus in the milk samples, but it does state that its belief that commercial, pasteurized milk is safe to consume has not been altered by these findings.
“To date, we have seen nothing that would change our assessment that the commercial milk supply is safe,” the statement said.
The document was long on assurances but short on details of what has been undertaken or found. It does not specify how many commercial samples were taken or in how many markets, nor does it indicate what percentage of the samples were PCR-positive for H5N1. The statement did not indicate if the testing suggested the amounts of viral genetic material in the milk were low or high.
Beef. From ABC, “USDA says it is testing beef for H5N1 bird flu virus“:
The United States Department of Agriculture said on Monday that it is conducting three separate beef safety studies. The agency is sampling ground beef purchased at grocery stores in states where dairy cattle have tested positive for the H5N1 avian influenza virus. It is also taking samples of muscle tissue from sick cows that have been culled from their herd.
Finally, they’re conducting cooking studies, which will inoculate ground beef with a “virus surrogate” and cook it to different temperatures to see how much virus is killed under each heat setting.
The move comes as one country, Colombia, placed restrictions on beef and beef products coming from US states where dairy herds have tested positive for avian influenza.
Now, I don’t especially like the idea of H5N1 permeating my comestibles. By the same token, however, if the effects were anything like other food supply issues, it seems to me that some illness would already have shown up (especially given the appearance of H5N1 in the media). Cholera H5N1 is not (at least, so far, not in food).
My concerns go to the possibility that the various agencies involved — USDA, FDA, CDC — are treating H5N1 as a food supply problem, and not as a potential pandemic breakout problem. For example, here is what APHIS is focusing on:
APHIS is strengthening its ability to quickly respond to significant animal disease outbreaks by announcing a final rule amending the animal disease traceability regulations and requiring electronic ID for interstate movement of certain cattle and bison. https://t.co/h0MUvPbr8I pic.twitter.com/VSTEildFQv
— USDA APHIS (@USDA_APHIS) April 26, 2024
Very well. But what about the humans in the CAFO operations? To be fair, it is true that CDC is recommending PPE (and training) for farmers and workers who might be infected by H5N1:
CDC: H5N1 in cattle – PPE recommendations
"Farmers, workers, and emergency responders should wear appropriate PPE when in direct or close physical contact with sick birds, livestock, or other animals; carcasses; feces; litter; raw milk"https://t.co/ow03ebjpvs pic.twitter.com/SE7SG63qST
— CoronaHeadsUp (@CoronaHeadsUp) April 17, 2024
(One notes the bitter irony that both cattle and workers in CAFOs will be safer than patients and HCWs in hospitals, at least if CDC’s profit-driven HICPAC gets its way.) But why on earth does CDC’s guidance stop at the CAFO door? Why is there no testing of the farmers and workers? From MedPage, “Are We Testing Enough for H5N1?“:
“We really need to be moving quickly to get our heads around what’s happening in the animal population and also what’s happening in the human population,” James Lawler, MD, MPH, of the University of Nebraska Medical Center’s Global Center for Health Security, told MedPage Today. “I don’t think we’ve been testing adequately to be able to get a real picture of that.”
Lawler said we should be particularly cautious “when a virus starts doing things that we don’t expect it to do, like circulating widely in a species where we normally haven’t seen infections. We really need to respect the potential danger that exists.”
Federal officials have confirmed that 33 dairy cattle herds in eight U.S. states have tested positive for H5N1. However, the outbreak is likely much larger than that, and has probably been spreading undetected for much longer than thought, Lawler said.
So we don’t really know how many humans are infected, do we? Farmers, culturally, don’t test:
(Many war stories online of farmers getting, say, an arm chewed up in a hay baler, binding themselves up, finishing the chores, and only then seeking medical help — quite possibly from the local veterinarian.)
Farmers also may have business reasons to evade testing. From the Daily Mail, “Large bird flu outbreak feared among Texas farmers – group shows symptoms of disease as experts warn cases are far more widespread than previously thought“:
Experts have warned that human transmission of bird flu may be far more widespread than thought, as farmers in Texas and Wisconsin are reported to have symptoms of the virus but are avoiding testing.
Dr Barb Petersen, a dairy veterinarian in Amarillo, Texas [the epicenter, remember], explained that workers at a local farm where cattle have tested positive for the virus are suffering tell-tale symptoms.
She said: ‘People had some classic flu-like symptoms, including high fever, sweating at night, chills, lower back pain,’ as well as upset stomach, vomiting and diarrhea.
They also tended to have ‘pretty severe conjunctivitis and swelling of their eyelids’.
Dr Keith Poulsen, director of the Wisconsin Veterinary Diagnostic Laboratory, told NBC News that he had heard reports of people with the infection.
He added that farmers are not cooperating with demands to test in part because of their long hours and because of fears they may be asked to cull their herds — as poultry farmers are to their flocks.
(I would imagine that any undocumented migrants working at the farms would also be reluctant to test).
Anyhow, here the testing that has been done. From MedPage once more:
In the current outbreak, at least 44 people have been monitored for symptoms, the spokesperson said, and more are being passively monitored, where they monitor themselves and report if they develop symptoms.
Overall, 23 people have been tested by states, with only one person — a farm worker in Texasopens in a new tab or window whose only symptom was conjunctivitis — tested positive, the [CDC] spokesperson said.
But see Barb Petersen, just above, for how ridiculous that result is. It’s almost as if CDC is afraid of what they might find? What’s wrong with testing as many humans in the dairies right now?
Finally, the institutional structure — CDC, USDA, FDA — is a big problem. MedPage once more:
CDC spokesperson said that while the USDA is responsible for livestock testing, the agencies are “working together to characterize virus specimens and monitor for changes that might make these viruses more likely to transmit to or between humans.”
“Working together.” Do you know what that means? It means no one agency is in charge of preventing a pandemic. That’s what it means. (More CDC hooey here[2]). A safe, or at least a profitable, food supply we understand. Pandemics, we don’t. We seem not to want to.
Pandemics and the Precautionary Principle
Readers will recall that Norman, Bar-Yam, and Taleb of the New England Complex Systems Institute (NECSI) published “Systemic Risk of Pandemic Via Novel Pathogens – Coronavirus,” in which they in essence called eveything that should have been done to control the current pandemic, none of which — this being the stupidest timeline — was done, on January 26, 2020 (!!).
The essential takeaway is The Precautionary Principle:
The general (non-naive) precautionary principle [3] delineates conditions where actions must be taken to reduce risk of ruin, and traditional cost-benefit analyses must not be used. These are ruin problems where, over time, exposure to tail events leads to a certain eventual extinction. While there is a very high probability for humanity surviving a single such event, over time, there is eventually zero probability of surviving repeated exposures to such events. While repeated risks can be taken by individuals with a limited life expectancy, ruin exposures must never be taken at the systemic and collective level.
That is exactly what “we” — CDC, USDA, FDA, and on up — are doing with H5N1: exposing ourselves once more to the risk of ruin at the “systemic and collective level.” (Osterholm’s “throw at the genetic roulette table”). We don’t even know how many humans are infected with H5N1, and it’s out there mutating in [checks APHIS chart] fifteen different species of mammal plus cows, besides humans (and, of course, our little dinosaurs, the chickens). Not only that, we don’t have even have a theory of how the stuff transmits (outside the milking unit at least). We don’t, for example, know if it’s being tranmitted because cows are fed poultry by-products.
NECSI’s concrete recommendations seem more tailored to SARS-CoV-2 than to H5N1 (perhaps some clever person will write an addendum for CAFOs). However, their general conclusion seems on point:
Standard individual-scale policy approaches such as isolation, contact tracing and monitoring are rapidly (computationally) overwhelmed in the face of mass infection, and thus also cannot be relied upon to stop a pandemic. Multiscale population approaches including drastically pruning contact networks using collective boundaries and social behavior change, and community self-monitoring, are essential.
Together, these observations lead to the necessity of a precautionary approach to current and potential pandemic outbreaks that must include constraining mobility patterns in the early stages of an outbreak, especially when little is known about the true parameters of the pathogen.
It will cost something to reduce mobility in the short term, but to fail do so will eventually cost everything—if not from this event, then one in the future.
Apparently, however, APHIS is constraining the mobility patterns of cattle. But not of people. CDC has nothing today about mobility patterns at all, nor do FDA and USDA. (It is easy to imagine a laid-off undocumented worker infected an entire homeless shelter in Houston or Chicago. It’s also easy to imagine farmers infectiing each ther where farmers gather: Feed stores, cattle sales, and so forth.
Conclusion
NECSI’s Norman et al., in their section on “Naive Empiricism,” warm against fatalism:
[A] common public health response is fatalistic, accepting what will happen because of a belief that nothing can be done. This response is incorrect as the leverage of correctly selected extraordinary interventions can be very high.
Here is a fine example, from — you guessed it — WHO:
Joint WHO/FAO/WOAH risk assessment. Risk to humans still considered low, but obviously the virus seems unstoppable https://t.co/DvsHiZ67bS
— Marion Koopmans, publications: https://pure.eur.nl (@MarionKoopmans) April 27, 2024
It’s not “obvious” at all, because we knocked other flus on the head in the early days of Covid with non-pharmaceutical interventions:
Maybe one of the most important graphs of the pandemic. Human behavior in Spring of 2020 crushed the spread of common pathogens. The idea that nothing can be done about endemic viruses doesn’t hold water. We should remember that with human to human transmission of H5N1 looming. https://t.co/WQPboSi7v2 pic.twitter.com/stTFSfS8BO
— Babak (@ChronicBabak) April 30, 2024
I suppose — [lambert pounds head on desk] — I will have to sally forth and attempt to induce a non-fatalistic attitude int others (after all, we’ve got wastewater testing now, which is good). Go thou and do likewise!
NOTES
[1] I’ve very weak on the clades, the various permuations of H*N*, so I’m not going there in this post. Here, however, is a good long thread on that topic:
2) We would first like to take a step back, and remember that the circulation of H*N* is an ancient story :
Fig. Possible origins of pandemic influenza viruses. Phylogenetic studies suggest that an avian influenza virus was transmitted to humans, leading to the 1918 pandemic pic.twitter.com/nkFSPdIgsX
— Emmanuel (@ejustin46) April 30, 2024
Key sentence: “Phylogenetic studies suggest that an avian influenza virus was transmitted to humans, leading to the 1918 pandemic.” Bird flu has form. It’s not something we want to mess around with or be lackadaisical about, though of course we hope for a good outcome, and not a second pandemic while we’re still suffering from the first.
[2] “CDC is committed to providing frequent and timely updates.” The page is dated April 19. No changes since then. This is, perhaps, the most entertainging of the many “We’re really doing something” bullet points:
• Designing an epidemiological field study and preparing a multilingual and multidisciplinary team to travel on site to better understand the current outbreak, particularly the public health and One Health implications of the emergence of this virus in cattle.
They don’t have their go-bags packed? Why aren’t they on-site already?


Wastewater testing… read the report this morning (FluTrackers)… 2 of 3 collection sites ( from what I read) had permitted “bovine” sources.. I am curious about the 3rd “liftstation, ie collection site”…haven’t seen any clarification on that 3rd site……
I like “risk of ruin” as a term of art that describes situations where a traditional cost-benefit analysis must not be used. That’s going into my personal vernacular.
There is nothing inevitable about contracting a virus like H5N1 or SARS-Co-V-2. The fatalism of the public health establishment and the propagation of Urgent Normal Syndrome, as Jessica Wildfire puts it, are the problems, and those two things are related.
Given the right marketing approach, wearing an N95 in public could easily become de rigueur. If I owned a significant stake in 3M I’d have the C-suite out on its ear for not taking advantage of this once-in-a-lifetime opportunity.
In the meantime, I’m going to keep taking care of myself and others by masking in public. I’m also unplugging from the meat/dairy/poultry industrial complex by eating vegan–at least for now. So far it’s been fun trying the different products out there and experimenting with new recipes.
Why does being a vegan equal trying different products? Do you mean factory-made food?
Only asking because my grand-niece is a vegan and she literally eats no real food. Veggies/fruit go in smoothie with chemical based protein pea powder. Everything else comes out of a box. Made by some ‘brand’ that is owned by food manufacturers’.
What am I missing please. Can you be a vegan and make your own meals from scratch?
It takes alot of work but I harvest my own garden and drive over to farms for chickens/eggs/honey and such.
PS I live in San Diego and ‘vegan’ trend is definitely over.
A box? Forgive me, it doesn’t seem very vegan. Most vegetarians, certainly the hardcore vegans, just want to avoid animal anything and probably prefer organic. I am a dedicated carnivore, but they make great food all the time. It just takes more work and there is the risk of getting vitamin B12 deficiency if you don’t take a supplement or eat something like dairy. Milk, eggs, cheese, or yogurt. A B12 deficiency must be avoided.
If you can cook, you can make homemade vegetarian meals. I can’t recommend any good cookbooks, but they do exist. Honestly, I am not a fan of salads, but a well prepared one seems more attractive than something in a box made by some corporation. God only knows what they put in it. The local grocery store or farmers market would be better.
My health has gotten better when I stopped buying the prepared food like stuff and make it from scratch because the FDA’s approval of any additives and substitutes, modern industrial food is unhealthy. Homemade is cheaper as well, unless you buy organic and pay the premium for it. Then it should equal out.
A couple of old vegetarian books:
Francis Moore Lappe’s book Diet for a Small Planet, and the cookbook by Ellen Buchman Ewald Recipes for a Small Planet based on Lappe’s work.
Also K2 and selenium.
I was a strict ethical vegan for 19 years and I did not eat processed food at all. Read Helen Nearing’s “Simple food for the Good Life.” One of the many reasons they had for being vegan was the simplicity of the food preparation. I stopped being vegan at about the time that all the processed garbage came out (I now also eat eggs and some fish and cheese). Anything can be turned into a way to sell junk; it may take discernment to realize that that is what is being done.
Most of the processed products I’ve tried are plant-based “dairy,” although I did buy a package of Impossible ground beef mostly out of curiosity. (It’s better in a bolognese/chili application than as a hamburger stand-in.) Lots of junk food is “accidentally vegan,” as they say, and I’m glad for that because it makes this undertaking feel less restrictive. By the same token, I’m not planning to eat Fritos, Oreos, or Skittles all day. A friend of mine gave me a book called Love & Lemons that has some wonderful looking recipes, and I will absolutely check out the book recommendations you’ve given me in this thread. Thank you!
From
UNMC
Nebraska Medicine
Global Center for Health Security
Is There a Vaccine for H5N1 Influenza?
“On the heels of a multi-state outbreak of highly pathogenic avian influenza A (H5N1) in dairy cows, experts told MedPage Today that a trio of H5N1 vaccines for humans has already been developed and approved in the U.S.
…
“If infections among humans who work with animals become more common, this could be a subgroup of people to vaccinate, he added. So far, only one human case in the U.S. has been reported this year.”
https://www.unmc.edu/healthsecurity/transmission/2024/04/24/is-there-a-vaccine-for-h5n1-influenza/
Looks like Dr. Bill thought of this ahead of time…(hmmmm) Where are the patent search folks?
https://www.gavi.org/vaccineswork/why-bird-flu-vaccines-need-urgent-rd
Dr. Bill is so prescient. / ;)
What’s the phrase? A self-licking ice cream cone? / ;)
I’ve got 450,000 Bessies down on the valley floor in Tulare County alone, and every last operation is of the CAFO variety, go big or don’t play.
We’re talking about 5,000 milk cows per operation, which means there is close to 100 mega-dairies, yikes!
An issue that didn’t exist before last year’s winter of record in the Southern Sierra, is the idea that Tulare Lake still has 1,000 acres of flyway for fowl play, and a good many of those CAFO operations aren’t far from the lake, what could go wrong?
I recall during the early days of the pandemic where a single person in Washington state tested positive. By that point “community spread” had already occurred, yet officialdom said otherwise.
I’m getting the same feeling here. If there’s been one there’s already others.
Time to stock up on toilet paper and N95 masks.
> I’m getting the same feeling here. If there’s been one there’s already others.
Quite right. Remember also that the Precautionary Principle urges that we shouldn’t assume that we can “catch up” by accelerating testing and tracing; exponential growth could already be occurring and we just wouldn’t know.
I’m sick for the first time since the pandemic started. Last Thursday I got together with two neighbors outside to chat. I had used Xlear, took a claritin and wore my Air Tamer – but did not wear a mask. On Sunday I woke up feeling lousy; wiped out and very slightly achy and very slightly warm intermittently.
I took a big blob of horse paste, a Metformin, three black cumin oil capsules, more claritin, my usual low dose methylene blue and more Xlear (NONE OF THIS IS MEDICAL ADVICE AND THE METHEYLENE BLUE CAN INTERACT BADLY WITH OTHER MEDS; SO CAN THE OTHER ITEMS). I felt lousy all day Monday. By this afternoon I felt close to normal. I tested negative on covid RATS on Sunday, Monday and today.
I am guessing this wasn’t covid (knock on wood); it felt like a regular virus. But I will keep testing for a while. The thing is, it could be avian flu. I eat dairy products. Who knows? And as a bonus, on Saturday night at 3 a.m. a bird got into our condo through our open patio door and it took us ages to get it out. Since when are sparrows awake at 3 a.m.? It seemed less energetic than I would have expected. We do have Influenza A showing up in the local wastewater (SF Bay area) presently, out of season.
Your best round up ever.
> Your best round up ever.
[lambert blushes modestly]
This is very kind of you to say, but I’m very conscious that institutionally H5N1 is more complex than Covid because of the involvement of multiple agencies. OTOH, with any luck, we’ll be in “at the birth” of a new pandemic!
I worry about the companion animal transmission because there is no federal agency with authority over companion animals (dogs, cats)
FDA regulates vet meds, and usda works with livestock but no one deals with companion animals.
Also I would say an outstanding question with the milking operations is if it’s fomites that get aerosolized because of the process rather then say actual airborne transmission. Then again at that point not a whole lot of difference to the person infected.
Especially because the H5N1 strain from cattle seems to be significantly more morbid in cats, from these case studies. The poor kitties died and before they died they appeared to go mad.
“Antemortem clinical signs in affected cats were depressed mental state, stiff body movements, ataxia, blindness, circling, and copious oculonasal discharge. Neurologic exams of affected cats revealed the absence of menace reflexes and pupillary light responses with a weak blink response.”
That’s an ugly constellation of symptoms and suggests some kind of cerebral and/or ocular trophism. Quite why cats should be so affected and cows not is mysterious. Man would appear to be somewhere in between, given the conjunctivitis reported, but where? More cat than cow or vice versa?
What’s the proposed mechanism for the virus making it through pasteurization in milk and still being active? Is it that it mutates to be (very) heat resistant? Or that occasionally we don’t fully pasteurize a batch of milk? Do any other viruses survive pasteurization?
> What’s the proposed mechanism for the virus making it through pasteurization in milk and still being active?
I haven’t heard of one. That’s why I think it’s a red herring.
Rummaging through the debris of half-remembered links, I recall seeing someone say that the fat in milk could protect the virus from the heat of pasteurization, and so was recommending purchase of low or fat-free milk.
And, I’ll add another good job, lambert high five.
Recent studies seem to show that all of the virus was inactive and they were unable to grow the virus in a lab.
I would stay away from non pasteurized milk and dairy products. well more so than usual.
Endemic Covid and epidemic, maybe pandemic, influenza both likely to mutate into deadlier, more infectious diseases. Lovely.
Is there any other diseases floating around ready for The Great Cleansing of Humanity? The pneumatic form of the Black Death, smallpox reborn, or a new, more easily transmissible, incurable tuberculosis? If nothing else, there are those defrosting corpses out on the tundra with their well preserved diseases. There must be something considering just how f—-ing stupid our medical system is as well as how democidal our leadership is.
I am slightly joking because dark humor can help, but I am serious about any other exciting new causes of mass death events. Something to put on my bingo card.
I’m still waiting for the Spontaneous Combustion pandemic to start! Won’t be able to hide that one.
🔥Poof!💨
Well, it would deal with the cremation. All the survivors would need is a vacuum.
I just might take up drinking again anyways while waiting for the rest of the Four Horsemen. I have been missing some of the Belgian beers.🍺
This is going to play merry hell with Lambert’s Water Cooler. Trying to keep track of one pandemic is enough but trying to keep track of two going on at the same time? That would be a nightmare.
> Trying to keep track of one pandemic is enough but trying to keep track of two going on at the same time? That would be a nightmare.
OTOH, now we can do “compare and contrast.”
New questions for “Would you rather..?”
Bacterial diseases tend to have a harder time causing pandemics in the modern world.
The Black Death in particular is pretty much a non-starter today given how it transmitted back then. There is a reason you still see outbreaks in Madagascar but it pretty much never spreads human-to-human in the Southwest USA, which is one of the main endemic regions, and not even in Bolivia, Brazil, Central Asia, etc. The modern city and modern sanitation just took the transmission routes out.
And in general, bacteria tend to have lower R_0 values (for various reasons having to do with physical size, infection mechanisms, etc.), thus spread slower, plus we (still) have antibiotics, etc.
Viruses are the main danger. And for most of them we still have to massively screw it up for things to spiral out of control because, again, they don’t spread that fast in most cases. SARS-CoV-2 was a perfect storm, and it was still eminently controllable, but we did botch it massively.
There isn’t really hard data to back this claim up, but based on the seasonal dynamics of regular flu and common cold coronaviruses, and of how past pandemics have gone, something like H5N1 should have zero chances to reach the super high R_e values that COVID did early on and when Omicron hit. So it should be much easier to control. At least in principle.
In practice we re in the post-COVID era, i.e. public health has been brutally gang raped and then murdered by the corporations and the financial oligarchy, and no longer exists. So anything can happen…
Would the immune dysregulation caused by Covid at scale theoretically make it easier for H5N1 to spread if it evolves to H2H spread, making the R_e higher than it otherwise would be?
And of course if you have gotten just enough covid to have damaged immune system function, then a bird-man-cow flu could affect you much worse than it would affect the never-covidized.
An excellent roundup. You can see all the pieces slowly coming together for the next pandemic and I see that the CDC and the WHO will handle that one as well as they are doing for the present one. Will they also argue that an influenza pandemic is also not spread by aerosol transmission but by not washings hands enough? The same factors which forced those two organizations to deny aerosol transmission of Covid i.e. cost of renovating buildings and making ventilation a priority, will still be in play for the next one. That is one helluva circle that they will have to square though as the bulk majority of people know exactly how the flu is spread. So, like the last time, we will be on our own once again.
“Cows aren’t washing their hooves enough” *rimshot*
“Cows should sneeze into their elbows.”
> An excellent roundup.
[lambert blushes modestly]
Covid at least one could not, it seems, get through food. Does H5N1 survive the human gastric tract?
I’m going to post a Twitter link, just because this random non expert guy seems to have a much better list of what we should be doing than any US agency has expressed.
https://twitter.com/PatientPersists/status/1784967211498500150/photo/1
Even Zeynep Tufekci (who has a spotty record on Covid, from what little I know) has apparently been tracking the H5N1 issue, and talking to officials for the past two weeks, says she is gobsmacked (see the whole thread I linked to).
This Twiiter guy also posts a link in his thread that says about 6 million Americans consume raw milk each week–a lot higher than I would have guessed. And I have not heard anything about the situation in other countries–are their dairy cows getting this?
There is a certain beauty to the notion that our fecklessness in responding to bird flu has ruined the food supply — both domestically and for export, a very big business — but I’m not sure there’s real reason to be concerned. Of course, there is an ick factor, which could cost the dairy and beef industries billions.
I assume the effects of food tranmission would be gastro, and we’re not hearing of any outbreaks, correct? (Raw milk is, I think, another matter, despite the ideologically commitments of some.) I do have strong priors on this but I think a mutation allowing much more efficient respiratory transmission — something that allows the virus to leap outside the CAFO — is the thing to watch for. Could be happening right now!
Adding, in retrospect, one reason SARS-CoV-2 was, in the aggregate, such an intelligent entity was that it preyed on so many of our weaknesses: Asymptomatic tranmission played upon our tendency to believe in the seen rather than the unseen, airborne transmission played upon our desires to congregate, and of course air travel was ideal. I am not sure what weaknesses H5N1 plays upon. To be determined, I suppose….
The Chinese, who were pretty much the only ones to do proper transmission chain tracking, found multiple well documented cases of SARS-CoV-2 transmission through fomites. Including, famously, through things like mailed letters.
That automatically means that transmission through food is a non-zero risk. It isn’t what happens in the stomach that is the immediate issue (although the virus does seem to thrive in the gut), it’s what happens while the food is in your mouth and throat. It depends on receptors and their distribution.
H5N1 would present a similar situation.
Of course the airborne route is the overwhelmingly dominant one and the main danger. But when you are trying to fully contain an infection, you have to pay attention to absolutely all possible exposure routes. The Chinese were trying to do that, so they documented fomite spread. We have absolutely no such intention, so we are going to allow milk and dairy products full of virus to be in every supermarket soon…
> It isn’t what happens in the stomach that is the immediate issue (although the virus does seem to thrive in the gut), it’s what happens while the food is in your mouth and throat. It depends on receptors and their distribution.
That’s a nasty twist of thought. I assumed gastro, but maybe it’s mutating toward receptors in the mouth and and throat even as we speak. That would be ugly, even if not respiratory. Boeing-level ugly (collapse of an industry, e.g. dairy) as opposed to Covid-level ugly (collapse of civilization).
As of mid-April, no cases yet in Japan. Detailed report (in Japanese) from NIID here:
https://www.niid.go.jp/niid/ja/diseases/ta/bird-flu/2621-cepr/12630-h5n1-riskassess-2404.html
There have been many HPAIV (H5N1) detection cases in birds in Japan — presently “the highest ever reported” —, and the NIID doesn’t rule out the possibility that it could become more infectious to humans.
Separately, the Ministry of Health, Labor, and Welfare announced today that they will stockpile the A/Ezo Red Fox/Hokkaido/1/2022 (NIID-00 2) vaccine, due to its antigenic similarity to the circulating virus strain.
Are the industrial pateurized milk herds and the artisan and artisandustrial raw milk herds sealed off from eachother in their two separate systems? If so, the bird-cow flu may not spread to these raw milk herds. Unless random birds spread it to them.
This one is going to end up as yet another laissez-faire capitalism-caused disaster, isn’t it?
We have endemic COVID now because the exploitative logic of laissez-faire capitalism was incompatible with a proper containment effort (i.e. shutting down travel, paying people to stay home and not work, having a properly organized state that can channel all the necessary resources into track-and-trace, mass testing, etc., these were all complete non-starters purely for reasons of political economy).
It’s the same factors at play in this case too.
What does the current situation call for?
1) Mass testing of all cows nationwide
2) Mass testing of the human population anywhere where the sewershed shows presence in the wastewater.
3) Cows are, if not culled, quarantined for a couple months until they test negative
4) Humans who test positive are also quarantined for a couple months
Rinse and repeat.
Is anyone doing that? Of course not. Some people are watching passively as the virus appears in wastewater and the milk supply, but other than that there is zero real action taken.
Why? Because somebody would have to pay for all the economic damage and to support the farmers, and that somebody would have to be either insurance companies (if there is even insurance against something like that), the state, or, most likely, the farmers themselves. The state cannot be bothered — sending hundreds of billions overseas to kill as many Russians as possible is its main current priority, who cares about H5N1 — which leaves the farmers stuck with the consequences. Those farmers naturally have all the incentives to not cooperate with containment if that is the case, plus many of them have been very successfully brainwashed into being fully ideologically committed to everything that stands against their real class interests, i.e. the exact last mindset you would want them to have in such a situation.
Perfect cluster**** once again.
P.S. The main article reports that there are likely a lot of human cases of H5N1 but does not mention anything about 50% of such people dying. This is a very important question to get to the bottom of. If there were hundreds of infections, presumably there would be dozens of deaths, and that should be noticeable. Alternatively, when it adapted to cows, it attenuated (but I don’t think people see any signs of that in the genomic sequences that have been released; although these things are rarely obvious). But even if that is the case, one should not relax, because if/when it picks up additional mutations to spread efficiently human-to-human, it may well deattenuate, in fact there is a certain evolutionary logic for it to do that.
> This one is going to end up as yet another laissez-faire capitalism-caused disaster, isn’t it?
Everything’s going according to plan (note that Taleb’s first step — limiting mobility — is exactly the step capital cannot take, and that Taleb argues it should be taken before ramping up testing is complete.)
I read something (I can’t remember what or where) regarding the “mildness” (such a weaponized word) of the H5N1 bovine infections. This person, who I seem to remember was knowledgeable on the subject, remarked that the main symptom for many of the cows was conjunctivitis and that the same was true in the known human cases.
This source then surmised that the virus had not yet mutated to acquire affinity for the lung tissue in mammals. So maybe, if this source is to be believed, the countdown is for the virus to evolve into a true respiratory disease in humans. Then, perhaps, you will see a lot of people start to die rather than merely coming down with a bad case of pink eye.
On the other hand, the infected farm cats went blind and mad then died. Perhaps pulmonary trophism is better than neuro-ocular trophism unless you want to live in Saramago’s “Blindness”.
It is not one or the other. It can easily be both.
And yes, the fate of the cats is very concerning.
But currently it does look like it has not adapted to efficient human-to-human spread, and when it does, that may well go together with a boost in the tropism in the wrong places, and then it’s “it was nice knowing you, everybody”. Maybe it won’t happen like that, but do we want to roll that dice?
Also, this is the moment to dust off some discussions from four years ago, such as the one about what fraction of critical workers can be taken out without society collapsing. With the huge caveat that likely nobody actually knows who is truly critical until those nodes in the network get taken out and it collapses. But some do seem obvious — power plant staff, key communication infrastructure maintenance people, etc., there are lots of places where just a handful of people know how to keep things going and if you lose them, you are out of luck. I recall those discussions during the early days of COVID, and the reason people were concerned about that aspect of the situation was that some estimates had it as low as 0.5% mortality leading to catastrophic loss of competency in the system. And early on the estimates for overall COVID IFR were several times that. In the end we didn’t see that problem manifest itself because of the combination of the extreme age skew in COVID deaths (meaning relatively low IFR in the younger cohorts) plus the relatively successful flattening of the curve plus vaccination. But with H5N1 there isn’t going to be such an age skew and a ton of working age people will die. So it doesn’t have to be anywhere close to 50% IFR to bring the apocalypse, even <5% may be sufficient…
> and the milk supply,
The thought occurs that if a fraction of the population comparable to the fraction that is concerned enough about CV to continue masking goes on a dairy products consumption strike on precautionary grounds (FDA/CDC/USDA assurances notwithstanding — who believes them anymore?), this will have an outsized effect on margins, the business being a commodity business.
It would be better to get way ahead of this for the sake of protecting consumer confidence in the safety of the product. “Pay me now or pay me later.”
I believe it has previously been noticed in posts and comments that these days “everything is Boeing.”
Aren’t most of those necessary measures precisely those that ended up being implemented to stamp out SBE (aka mad cow disease)? Systematic testing of animals, large-scale culling, testing of suspected cases amongst human beings — and ultimately, prohibition of feeding ruminants with animal carcasses processed into some kind of flour.
Of course, before all that took place, mad cow disease and its associated variant Creutzfeldt–Jakob disease (definitely not “mild”) in human beings had spread uncontrollably.
I wonder if anyone has tested swine heards. I think there are old studies (15 years ago) showing that h5n1 in Asia was often asymptomatic in swine. It is hard to imagine it not being in swine unless it really is spreading mainly through the milk transmission and cow feces route.
I’m more curious about the feral pigs. H5N1 has been detected in two states with extensive feral swine populations, Texas, and North Carolina. But hard to imagine it’s not in California too. My guess is they may have more exposure to cattle than domestic pigs in CAFO.
USDA-APHIS routinely samples all feral pigs removed in damage control operations. I’m pretty sure avian influenza was on the list of things they tested. If not, guessing it is now.
CDC paper from 2022 on spillover risks from H5N1 in swine.
https://wwwnc.cdc.gov/eid/article/30/4/23-1141_article#:~:text=Mammalian%20adaptation%20and%20reassortment%20may,previous%202%20centuries%20(1).
This doesn’t surprise me. After watching the the CDC, the FDA, and the Medical/Hospital industry these past 4 years I think their financial incentives are not aimed toward improving public health in the US. Just the opposite. I’m as frustrated by this as anyone. At this point I don’t expect anything different. If nothing else this lack of expectation keeps me from banging my head on the desk wondering why the CDC and FDA seem so incompetent or indifferent… or worse.
This utube doc. came out 3+ years ago early in the pandemic. Nothing has changes as far as I know. This video is largely forgotten now, lost in the ongoing rush of “crisis” events. It’s worth watching, imo. ~1hr 10 minutes.
Perspectives on the Pandemic | The (Undercover) Epicenter Nurse | Episode Nine
https://www.youtube.com/watch?v=UIDsKdeFOmQ
What does that video have to do with this story?
Federally guaranteed financial rewards for certain actions regardless of outcomes. etc. And if those actions’ outcomes are challenged as insufficient or even subpar?
Where is the Fed govt’s true interests?
Setting aside the tendentiousness of the video in question, if the motive of the (any) federal government were really to give away money to undeserving institutions, there are far simpler, more reliable and considerably less risky ways to do that than by way of onboarding a pointless and avoidable pandemic that does, in fact, kills millions of people worldwide, causes immense morbidity issues that are a perpetual drag on the labour that needs to be exploited (drags so obvious that even Larry Summers can notice them), and annoys everyone else by temporarily halting commerce, tourism, dining out etc. That was true in 2020, and would be true of any potential 2024/25 H5N1 pandemic.
One wonders how much “incompetence” at CDC and FDA was created by imposing a layer of censorship-imposing and career-punishing/destroying political-business commissars on top of all the scientists and technicians.
In the lhe last go-round of avian flu, ca. 2015, I happened to be conducting aquifer tests in MN farm country. At that point the mechanism of spread of that flu virus was unknown, and I don’t think anyone has solved that problem since, so each farm we visited we had to disinfect our boots.
One thing we (my team and I) noticed, and was hard to miss, is that the local turkey and chicken farmers tended to move dead poultry out of the barns and into piles outside for later disposal. These carcass piles, while they were there, were feeding enormous amounts of wildlife, most notably many scores of bald eagles. When the trees are crammed full of bald eagles, especially when miles away from open water in December and most of the terrain is cornfield, you really can’t forget it. We reported the observation to the MN DNR and Ag Dept., but as far as I know nobody looked into whether or not scavengers, especially eagles, we’re a vector. For that matter, no explanation for flocks of 100+ eagles in Minnesota cornfields was offered.
Cows should keep six feet apart and avoid crowded and close environments.
Will do wonders for ending CAFO’s :-)
On many of the CAFO operations in Godzone, you’ll see a strip of grass just beyond the crowded enclosure, family-blogging with the Bessies.
maybe we should also point out that bird flu in cattle was way lower during Trump’s era.
???
Well, lets re-elect Trump and that bird flu in cattle will go right back down to where it was during Trump’s era.