Yves here. Even though this article is for the most part highly informative, it seems to be unduly inclined to take the point of view that there must be biomarkers, a well-understood pathological process, and/or a tidier set of symptoms. It seems to be a lapse this piece does not even mention chronic fatigue syndrome. For many years, patients who suffered from it were treated as being hypochondriacs or having some other psychological ailment. The two people I knew personally with chronic fatigue were high energy, highly respected professionals with good personal relationships. And there were no obvious triggers for their onset of chronic fatigue.
So it strikes me as medical researcher arrogance to think they can or should be able to get their arms around a new set of pathologies quickly, when there are many that have been around for a long time that we still don’t understand well, from sudden infant death syndrome to Alzheimers to chronic Lyme disease (which some medical professionals claim does not exist).
By Sara Talpos, a contributing editor at Undark. Originally published at Undark
In January, the physician-scientist Ziyad Al-Aly delivered a harrowing message to a U.S. Senate committee. Eyes wide, eyebrows lifted above a tan face mask, he catalogued the body parts at risk of damage from long Covid: the brain, the heart, the gut, not to mention hormones and the immune system. The condition strikes the young and the old, he warned, and one’s personal risk never goes away. “Even if people emerge unscathed after having the first infection,” he told the Senate, “they can still get long Covid after reinfection.” Recovery rates are low, he continued, and without prevention and treatment, the disease’s burden will continue to mount.
From positions at Washington University in St. Louis and at the Veterans Affairs St. Louis Health Care System, Al-Aly has emerged as one of the world’s most cited experts on long Covid. He and his colleagues at VA St. Louis have published in prestigious journals, and online biographies suggest that Al-Aly has served on several U.S. government committees, as well as a high-profile panel that looked at how long Covid can impair a person’s ability to work or attend school. In May, Time named him one of the 100 most influential people in health.
That influence has made Al-Aly and the VA St. Louis group standard-bearers for a particular view of long Covid, one shared by many clinicians and public health officials. It frames the post-viral condition as encompassing hundreds of symptoms and diseases and posing a significant threat to the United States. Speaking to the Senate committee, Al-Aly said that at least 20 million Americans suffer from long Covid; the condition, he added, has caused as much disease and disability as cancer and heart disease.
Al-Aly has earned praise for bringing much-needed data to an underrecognized condition. His studies reflect “what I and my colleagues see on the ground in clinical practice,” said Svetlana Blitshteyn, a neurologist and director of the Dysautonomia Clinic in Buffalo, New York. The cardiologist Eric Topol, an occasional Al-Aly co-author and director of the Scripps Research Translational Institute, called Al-Aly’s work with VA data “as good as it gets.” And Al-Aly has become a go-to expert for the disease, presenting his views about the threat in numerous news articles and opinion pieces.
Few experts dispute that long Covid can be debilitating, or that it warrants careful study. But in interviews with Undark, a number of experts said that it is misleading to frame long Covid as an increasing threat. The best data, they say, suggest that most people recover from the disorder and that long Covid rates will decline as people develop immunity. (A July study by the VA St. Louis team also found that rates of long Covid declined over the course of the pandemic.)
The work produced by Al-Aly and his colleagues, which relies on electronic health records of U.S. veterans, is also a key point of contention. In interviews, several experts questioned the VA St. Louis’ methods. At the request of Undark, Harvard epidemiologist Marc Lipsitch reviewed the group’s first long Covid study and raised a range of concerns. Many of them related to the handling of negative controls, a statistical technique that, when deployed properly, can help researchers detect problems in the analysis of their dataset. Some of the negative controls “are simply misused in the paper,” Lipsitch wrote in an email to Undark.
Additionally, some experts suggested that the VA St. Louis studies are not truly measuring long Covid. “They’re not studying post-viral illness, in my opinion, in these VA studies,” said Anders Hviid, a professor at the University of Copenhagen and head of the Department of Epidemiology Research at the Statens Serum Institut. Post-viral syndromes, said Hviid, are relatively rare and are usually characterized by fatigue and cognitive difficulties. Al-Aly’s research, meanwhile, looks at what Hviid described as a gamut of outcomes: dementia, thromboembolisms, psychiatric diseases, kidney diseases — “everything under the sun,” he said.
At best, the studies are detecting health problems known to occur when people with poor baseline health experience a severe infection of any kind, said Hviid. At worst, the findings simply reflect bias in the study design, and are picking up on symptoms that are not caused by Covid-19 at all. “It’s a disappointment that not more U.S. scientists have spoken up about this,” said Hviid.
The differing viewpoints stem in part from the difficulty of studying a disease that doesn’t have a known biomarker — something measurable in the body’s fluids or tissues that can distinguish patients with long Covid from everyone else. Instead, many researchers have turned to data from medical records and surveys. But the process of gathering and interpreting such data is not straightforward. To date, studies have yielded vastly different answers to seemingly basic questions, including the number of people living with long Covid and the likelihood of recovery.
Between these deep divisions are long Covid patients desperate for clear answers. These patients, Al-Aly suggested in a series of interviews with Undark, are a central motivation. The VA St. Louis findings have been peer reviewed and reproduced in various settings, Al-Aly said, and he pointed to what he views as severe limitations in some studies that have yielded results that run counter to his own. He also cautioned that an overly narrow definition will exclude some patients from research and medical care. “We favor a more inclusive approach,” he said. (Al-Aly did not directly respond to a list of emailed questions about his team’s use of negative controls, or to what some experts suggested were other methodological inconsistencies in the team’s research.)
An inclusive approach to long Covid was recently recommended by a report published in early June by the U.S. National Academies of Sciences, Engineering, and Medicine, which advised physicians to consider a long Covid diagnosis with any new or worsening symptom or disease lasting at least three months and occurring after a SARS-CoV-2 infection. The report did not state specifically how much time might elapse between the Covid infection and the appearance of long Covid.
According to some researchers who spoke with Undark, the report’s broad definition rests on shaky evidence, could complicate clinical trials, and may end up trivializing long Covid. But Al-Aly, who served as a reviewer of the National Academies report, said that the challenges of using a broad definition can be addressed through sub-phenotyping, or the clustering of patients based on symptom patterns. One way to think about this, he said, is to look at the history of cancer: Initially every lump was simply viewed as a tumor, but as science evolved, researchers learned to differentiate between hundreds of different cancers.
Taking this broad approach to long Covid, he suggested, is “really the right thing” to do.
Almost from the start, long Covid proved vexingly difficult to measure and track. Early on, researchers would survey people in the months after a Covid-19 infection and ask if they were experiencing symptoms like fatigue or shortness of breath. Most said yes: A systematic review analyzing papers published during the pandemic’s first year estimated that nearly 75 percent of people developed at least one persistent symptom, or what could now be considered long Covid. That figure “just doesn’t pass the sniff test,” said Michael Putman, a rheumatologist and research methodologist at the Medical College of Wisconsin.
The problem, said Putman, is that symptoms like fatigue are extremely common, including among people who had not caught Covid-19. Those early studies were picking up on lots of symptoms that had nothing to do with the virus, in addition to some actual long Covid cases.
In order to figure out which symptoms are connected with a Covid-19 infection, researchers need to create a comparison, or control, group comprised of people who have not yet been infected. But many of the earliest long Covid studies didn’t do this. “There’s a lot of research that was done very poorly, that has seeded the literature with nonsense,” said Putman.
Al-Aly was part of a wave of researchers who launched more ambitious studies, with control groups, in an attempt to get a better handle on the scope of long Covid. In a recent interview with Undark, Al-Aly recalled a March 2020 Zoom call with his team at the VA. “We saw the world in crisis, the house on fire,” he said. “What do we do — do we sit by the sideline and chew gum and watch TV and watch TikTok?” His team wanted to pitch in by identifying key unanswered questions to study.
Not long after the meeting, people began showing up in clinics, said Al-Aly, sometimes weeks after an initial infection, reporting that they had not fully recovered. They were struggling with a range of symptoms, including fatigue, brain fog, shortness of breath, and persistent coughing. Patients were also finding each other online, and by the summer of 2020, they had coined and adopted the term long Covid to describe their condition. Here, said Al-Aly, was an issue that the public cared about — and that his team could help with.
They had access to an incredible trove of data: the electronic health records for millions of patients in the VA system. Al-Aly had previously used VA data to study the health effects of air pollution and to identify potential side effects of common medications. This earlier research was like a rehearsal, he said, one that prepared him to respond to the pandemic.
He and his colleagues soon launched their first long Covid study. They took a group of more than 87,000 VA patients who had tested positive for Covid-19, and then compared their health records with those of a control group with no record of infection. As it turned out, people who had caught Covid-19 were likelier to die in the six months following their illness than people who had never tested positive. Their health records also showed that, in the months after catching Covid-19, they registered a range of diseases, symptoms, and prescriptions, including for opioids and antidepressants, at higher rates than people who didn’t have a documented case of the illness.
The study additionally found a now well-established pattern: Patients who had spent time in the intensive care unit, or ICU, were at higher risk than those who had been hospitalized but had not been admitted to the ICU. Those who had not been hospitalized at all were at the lowest risk of persistent symptoms.
The paper was published online in April 2021 in the journal Nature and received widespread media attention. “‘Long Hauler’ Study Shows Covid Can Kill Months After Infection,” read one headline.
The VA team followed up with more studies. One 2022 paper found that patients with a documented Covid infection had elevated rates of neurologic diseases, including stroke, depression, and anxiety, as well as movement and cognition disorders. The paper itself noted that the research was conducted mostly in White men, which may limit its ability to speak to the wider population of Americans. That nuance, though, was lost in a press release from the Washington University School of Medicine in St. Louis, which extrapolated the study’s findings to the entire U.S. population, warning that 6.6 million people “have suffered brain impairments associated with the virus.”
At a time of pitched battles over Covid-19 policies, such eye-catching claims found an audience. Al-Aly’s work propelled him into the public spotlight, where he used his platform to sound an alarm: Long Covid was a public health crisis and its effects would have a profound and lasting effect on large swathes of American society. In a 2021 interview with Bloomberg, Al-Aly warned about deteriorating mental health: “Let’s not act surprised two years down the road, when people start committing suicide.”
“We’re seeing brain problems in previously healthy individuals and those who have had mild infections,” Al-Aly told Psychology Today in September 2022. “It doesn’t matter if you are young or old, female or male, or what your race is. It doesn’t matter if you smoked or not, or if you had other unhealthy habits or conditions.” About a month later, in The Washington Post, he compared the risk of a second Covid infection to the risk of playing Russian roulette.
But even as Al-Aly was becoming a public figure, other experts were looking at his methods and raising questions, including a basic one: Should all of these symptoms and conditions — obesity, pressure ulcers, urinary tract infections, asthma — really be considered long Covid?
For more than a century, physicians have known that viral infections are sometimes followed by mysterious, long-lasting symptoms. But defining those illnesses has been a persistent challenge.
In contrast to a well-defined disease like cancer, there’s no blood test or imaging technique that can reliably differentiate people with and without a post-viral illness. Instead, researchers collect data on symptoms and then use the results to create what’s known as a case definition: a set of criteria that allow clinicians and researchers to determine whether someone does or doesn’t have the condition.
In the fall of 2021, the World Health Organization adopted a long Covid case definition. According to the WHO, anyone with a symptom that persists or develops three months after an initial Covid-19 infection, and that can’t be otherwise explained, could be described as experiencing long Covid. Soon after, a group led by Terence Stephenson, a pediatrician and professor of child health at University College London, developed a similar definition for adolescents that could be used for research purposes.
To arrive at its definition, Stephenson’s team gathered researchers, along with parents and caregivers, and then used a consensus approach. There was some tension in the process, said Stephenson. Parents and caregivers felt that one life-altering symptom should be enough to constitute long Covid; whereas researchers and clinicians wanted to limit the diagnosis to patients with more than one serious symptom. The parents and caregivers won the debate. “We ended up with what I would call a very permissive definition,” said Stephenson, who said he stands by the consensus process. (A version of the definition was ultimately adopted by the WHO.)
A 2023 study points to the potential problems with a broad case definition, however. The study used the WHO definition to evaluate 467 people ages 12 to 25 who received a Covid test. The study participants were evaluated early on and then again at six months. As it turned out, nearly half the people who had Covid-19 would meet the WHO criteria for long Covid — but so would nearly half the people who had never been infected with the virus.
The study’s lead author, Joel Selvakumar, a pediatrician and Ph.D. student researching long Covid at the University of Oslo, said the findings generated a polarized response on social media. That’s because of what he characterized as two strident groups with opposing views: One thinks Covid is a hoax, while the other thinks researchers and governments are covering up the disease’s severity. The polarization seems especially intense in the U.S., he observed, and it obscures the underlying issue: At least for studies like his, the current case definition is unreliable.
Unlike Al-Aly’s studies, Selvakumar’s study excluded hospitalized patients. That’s partly because young people are rarely hospitalized due to Covid, he said, but also because any lingering symptoms might be caused by a different underlying mechanism, such as direct tissue damage from severe infection.
Symptoms that develop post-infection are not always due solely to the infection itself. Hospitalization for any reasonincreases a person’s risk for a wide range of medical problems after discharge. Such problems may have little to do with the initial diagnosis and instead stem from the stress of a hospital stay: The disrupted sleep, poor nutrition, and lack of exercise can all contribute to the onset of new health problems. Additionally, people who are very sick do not always fully recover, and their lingering symptoms are often not specific to the initial illness.
“We have names for those syndromes already,” including post-intensive care syndrome and post-hospitalization syndrome, said Anil Makam, a hospital medicine physician at the University of California, San Francisco, who studies patients in long-term acute care hospitals, where many patients go after an ICU stay. Makam recently published a studythat used validated surveys as well as interviews to understand the long-term outcomes of patients who were hospitalized with the most severe cases of Covid-19. His study didn’t have a control group, he said, but the results echo what was known before the pandemic: The sicker the patient, the more likely they are to have persistent multisystem disabilities.
It doesn’t make sense to conflate these conditions with long Covid, he said. Lumping everything together leads to a distorted view of long Covid, and it could complicate efforts to understand the underlying mechanisms and identify possible interventions. “You’re just going to be on a wild goose chase to find treatments,” he said.
Some experts said a broad definition could be useful in the context of public health and epidemiology. Sharon Saydah, an epidemiologist at the Centers for Disease Control and Prevention, said that when CDC scientists crafted the agency’s long Covid definition, they wanted “to make sure we’re not missing anything, that we’re including everyone who might be experiencing ongoing symptoms or new conditions” related to a Covid-19 infection. In a 2021 opinion piece for The Guardian, Al-Aly criticized the WHO’s definition for excluding new onset diseases, such as diabetes and heart disease, which his own studies have detected. These new conditions should count as long Covid, he wrote; otherwise, governments may fail to prepare for “the tide of patients with these chronic conditions.”
(In an email to Undark, a WHO spokesperson, Tarik Jasarevic, wrote that its definition may include new onset disease: The definition “focuses on symptoms but doesn’t specifically exclude new onset disease. New onset conditions like diabetes, lupus, stroke, etc. may be considered” long Covid, Jasarevic wrote.)
At stake, Al-Aly suggested, is a broader struggle: That of long Covid patients who seek to have their symptoms taken seriously, but may encounter skepticism from peers, employers, and caretakers. “I worry that this myopic definition of long Covid may be used by governments and health insurers to debase the disease and deny insurance coverage,” he wrote. “It may add fuel to the gaslighters’ fire, providing them with a moral license to sow more skepticism around the existence of this disease.”
In an interview with Undark, he said that for too long post-infectious illnesses were marginalized. Then, when pandemic hit, the health care system was caught flatfooted. There is no national medical society to champion patients’ cause, and individual physicians are unsure about how to help, he said. Congress allocated more than $1 billion in 2021 to fund long Covid research (and the government kicked in an additional $515 million this year). That’s a start, said Al-Aly. But it’s nowhere near enough.
In the spring of 2021, after Nature published Al-Aly’s first long Covid paper, Anders Hviid’s first reaction was surprise. Nature is a top journal, but it was unusual for the publication to feature epidemiology, said Hviid. Even more unusual were the study’s findings. “It’s just difficult to imagine that a simple respiratory virus could be so detrimental to all organ systems at a population-level scale,” said Hviid. One’s intuition can always be wrong, he added, but given that other respiratory infections, including influenza, do not exact such a massive toll, skepticism seemed like the right starting point: “You should question, ‘Can that be right?’”
For more than two decades, Hviid has conducted research using Denmark’s centralized medical records. During the pandemic, he and his colleagues used electronic health record data to conduct vaccine safety and effectiveness studies. And by late 2020, he had also turned his attention to long Covid, securing funding for a study that would survey the Danish population about their post-Covid symptoms. Such questionnaires offer fine-grained data that can be difficult, if not impossible, to obtain through electronic health records, said Hviid. Nevertheless, Al-Aly’s study had piqued his curiosity. He decided to conduct EHR-based studies as well.
This February, he and four colleagues published a study using medical records of the entire Danish population aged 12 and over. In contrast to Al-Aly’s work, that study found no evidence of substantial neurological or psychiatric symptoms in non-hospitalized individuals one year after a Covid-19 infection.
A defining feature of the study, said Hviid, is its high number of mild or asymptomatic infections. These were documented thanks to the country’s widespread surveillance testing. People getting tested in Denmark were often young and healthy. They got tested because it was a requirement for socializing.
Hviid’s team did see a meaningful increased risk of persistent symptoms among those who had been hospitalized. “That’s not particularly surprising,” he said. A severe course of any illness can lead to lingering effects.
Hviid and his colleagues aren’t the only researchers to find that long-lasting Covid-19 symptoms are rare for people with mild illness. A 2023 study looked at the electronic health records of a nationally representative sample of Israeli citizens with mild cases of Covid-19. It found that they were “at risk for a small number of health outcomes.” But most of the symptoms resolved within a year.
That study “confirms the statements that we’ve made that by and large, by one year, most people will have recovered,” said Theo Vos, an epidemiologist who helps track long Covid for the long-running Global Burden of Disease study.
Vos is an author of a 2022 systematic review that pooled data from 54 studies and two medical records databases, then grouped study participants into three symptom clusters: one centered around fatigue, another around cognition, and a third around breathing problems. The authors found that, among non-hospitalized people, just 0.7 percent had not recovered by 12 months after infection. This compared with 11 percent of those who were hospitalized and around 20 percent of those whose hospital stay involved the ICU.
In an April email, Selvakumar pointed out that many early long Covid studies were conducted on non-immune populations. That’s important to keep in mind, he wrote, because “the largest risk factor for long Covid is initial severity.” Thanks to immunity from vaccines and prior infection, most people today are less likely to have a severe course of the illness — thus, their risk of long Covid has declined as well.
Comparing an Al-Aly study of mental health outcomes with Hviid’s offers a glimpse into the dizzying number of variables that can influence a study’s results — even when, on the surface, the studies appear similar.
“There are huge differences” between the two studies, said Jeffrey Morris, director of the Biostatistics Division at the University of Pennsylvania’s Perelman School of Medicine. He started ticking them off: different study populations, different designs, different time periods.
Both approaches, Morris said, had merit.
Other researchers agreed that Al-Aly’s studies have merit, but stressed that the work is limited in its ability to speak to long Covid in the broader population. As a group, VA patients are older and less healthy. As a result, they are at higher risk of severe infection that might lead to hospitalization or even a stay in the ICU, events that increase one’s risk of long Covid. The VA studies look at “a very special group of high-risk people,” wrote Selvakumar in an email, “so you have to be very careful when extrapolating to the general population.” While a given study may note this limitation, he continued, the caveat sometimes gets lost in what he characterized as media spin.
One researcher doing similar studies was cautious about extrapolating his findings to the broader population. Junqing Xie, a post-doctoral researcher at the University of Oxford, recently co-authored a paper that used data from the U.K. Biobank to look for a connection between a Covid infection and psychiatric disorders and prescriptions. Similar to the VA team, Xie’s team found a link. However, it’s unclear what precisely this means for the general population, said Xie. “We are not able to infer any prevalences,” he told Undark. To do that, a researcher would need to ensure that their study participants are highly representative of the broader population. Neither the BioBank nor the VA databases meet this criterion, he said.
Within the already-less-healthy VA population, some experts said, Al-Aly’s infected groups probably skew toward more serious Covid-19 cases. That’s because people with asymptomatic or mild cases are much less likely to visit a doctor, who would then document the positive result in the patient’s electronic record. The effect would have become increasingly pronounced as time wore on and people developed immunity and started testing at home, said Makam. He pointed to a VA study that looked at the risk of organ damage associated with reinfection. People with multiple Covid infections documented in their health records probably had relatively more severe courses of illness, he said. This doesn’t mean that the average person who gets reinfected and can manage their illness at home is at heightened risk of organ damage.
(The study, published in Nature Medicine, doesn’t mention this as a limitation, though it does suggest that bias could run in the opposite direction: If people with Covid-19 don’t get tested, and if they are at heightened risk of bad outcomes, then they could make the uninfected group look sicker than it actually is.)
Some experts also raised concerns that the VA St. Louis team has worked with data in ways that, from the outside, don’t clearly map onto established statistical practices.
In his email, Lipsitch raised questions about the group’s use of negative controls, a statistical technique that can help a researcher determine whether any associations — for example, an association between a Covid-19 infection and smell loss — are causally linked.
In an influential 2010 paper, Lipsitch and his colleagues proposed that negative controls should be routinely deployed in epidemiological studies. Applied to the study of long Covid, one type of negative control, called a negative outcome control, might involve identifying health conditions that are highly unlikely to be caused by the infection: accidental injuries, for example, or scarring. If an infection were found to be associated with one or more of these unrelated conditions, then this would suggest that some other variable — something other than the Covid-19 infection — is influencing the study’s results.
In order for this technique to work, said Lipsitch, researchers need to define their negative outcome controls before they conduct their analysis, and then report all the findings. The VA St. Louis’ first paper used neoplasms — a medical term for tumor — as a negative outcome control, but in the preprint, neoplasms were not treated as a negative control; rather, they were treated as an ordinary outcome. “There are also issues about how the negative outcome controls were chosen in subsequent papers,” Lipsitch wrote to Undark. The negative outcome controls differ across studies, he said, and it’s not clear why.
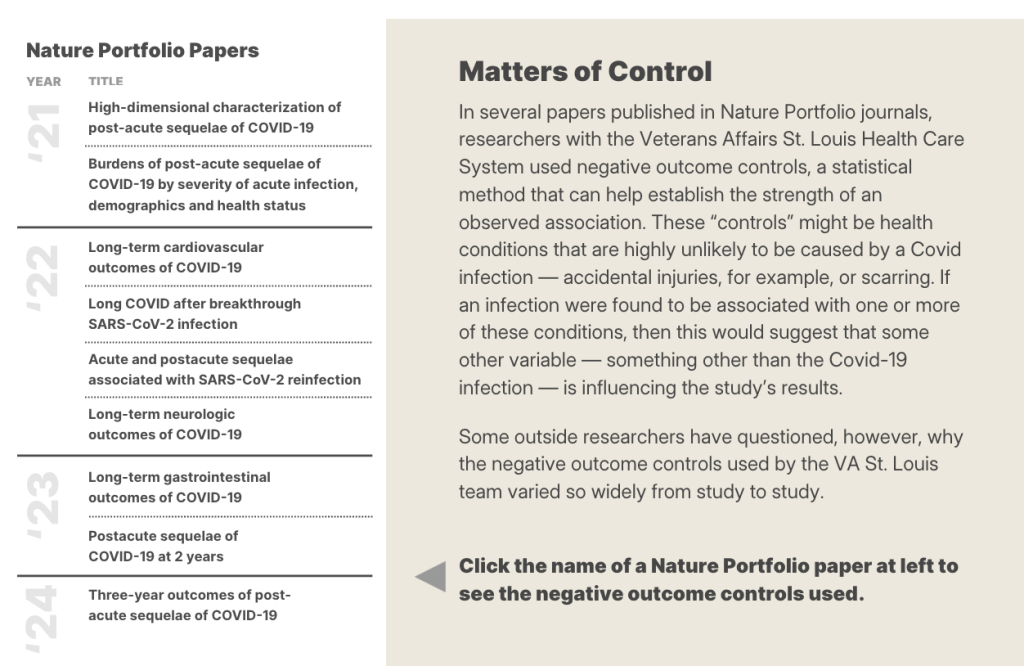
Some of this is difficult to parse, Lipsitch said, because the study’s methods are not clearly explained. “I think this is a case where peer review didn’t do its full job,” he said. “Because part of what peer review should do is to ensure that people with expertise in the field, ideally can reproduce, but at least can understand — in detail — what was done and make a judgment of how valid it was. And in this case, in its wisdom, Nature decided to let through a series of papers that describe their methods in such vague terms that it’s really hard to know what was done.”
Hviid also noted that the VA team changes its negative controls, along with its comparison groups, from study to study. “It’s a little bit weird,” said Hviid. Ideally, a research team would establish its analytical setup and then, whenever it wanted to add more data, the team would rerun the analysis using the same design. “I’m not saying that they’re intentionally fraudulent,” Hviid added, “but you’ve really got to be careful as a researcher if you’re sitting and running a lot of different analyses.”
The VA St. Louis team also used different approaches — including different weighting methods and a regression adjustment — to make its Covid and non-Covid groups comparable.
There might have been valid reasons for a research team to make such changes, experts told Undark. Peer reviewers might have requested them, for example. When asked about this by email, however, Al-Aly did not provide a rationale.
Undark also shared many of these concerns in a detailed email to Nature, whose portfolio journals published nine of the VA St. Louis’ long Covid studies. In response, Isobel Lisowski, a communications officer for Springer Nature Group, forwarded a statement on behalf of Nature Portfolio, which she asked to be attributed to Magdalena Skipper, editor-in-chief of Nature: “Our journals are editorially independent of each other, and each paper is assessed and peer reviewed independently based on its own individual merits. At all times our commitment is to ensure the accuracy of the scientific record and, if concerns are raised with us directly, we look into them carefully.”
The statement further noted that the VA St. Louis papers used several approaches to test the robustness of the findings, and that a reporting summary was published with each paper to increase transparency.
The BMJ, which published the VA St. Louis’ paper on mental health outcomes, published notes from the peer review. The reviewers did not raise the topic of negative controls. The VA St. Louis team did indicate that it was building additional cohorts to address reviewers’ concerns about possible bias in the study design.
Al-Aly is not unaware of the criticism. “I love these questions,” he said, wrapping up the first interview with Undark, during which he discussed his research as well as its possible limitations.
In conversation, Al-Aly is warm and funny, peppering his sentences with colorful idioms and playful hyperbole. (“You could test your cat if you wanted to. You can test your dog,” he said, recalling how Americans initially went all-in on at-home Covid testing.) He’s also willing to brawl, at times suggesting that many of his critics lack the expertise to evaluate his work or produce good research of their own. “We get a lot these newbies. They want to do studies,” he said. But their work sometimes contains what he characterized as “sophomoric mistakes.”
One example, in his view: the 2023 Israeli study of people with mild symptoms, which was published in the BMJ. “Do me a favor and look at their Figure 7,” said Al-Aly, off the top of his head, when asked about the paper.
Al-Aly pulled up the study on screen. Figure 7 shows that the vaccinated individuals in the study were at a higher risk for memory problems than the unvaccinated. The most plausible explanation, said Al-Aly, is that the researchers haven’t fully accounted for bias in their dataset. Further, he said, the study seems to assume that if a diagnostic code stops appearing in a patient’s medical record, this means the condition has resolved. In reality, said Al-Aly, “it’s very hard to document the resolution of symptoms in EHR.”
(In an email to Undark, a study co-author, Maytal Bivas-Benita, said that the memory finding wasn’t statistically significant. She added that her group’s findings are supported by a more recent Israeli study, which found a return to baseline in medication use and health care costs in non-hospitalized Covid-19 patients.)
Al-Aly was also critical of the study from Hviid’s team. Their control group, he suggested, consists of people who tested negative. The distinction matters because during the pandemic people with worse baseline health tended to test more frequently. A cancer patient needing chemotherapy in 2020, for example, would first need a negative Covid test. “When you compare sick people to sick people, you’re not going to find big differences,” said Al-Aly.
Speaking about the Danish study, Al-Aly said, “it’s not unreasonable to even call it deeply or fundamentally flawed.”
(“Clearly he has not read the paper very carefully,” said Hviid. His team’s control group included everyone without a positive test. While they did perform an additional analysis with a test-negative control group, Hviid said, it yielded the same results. )
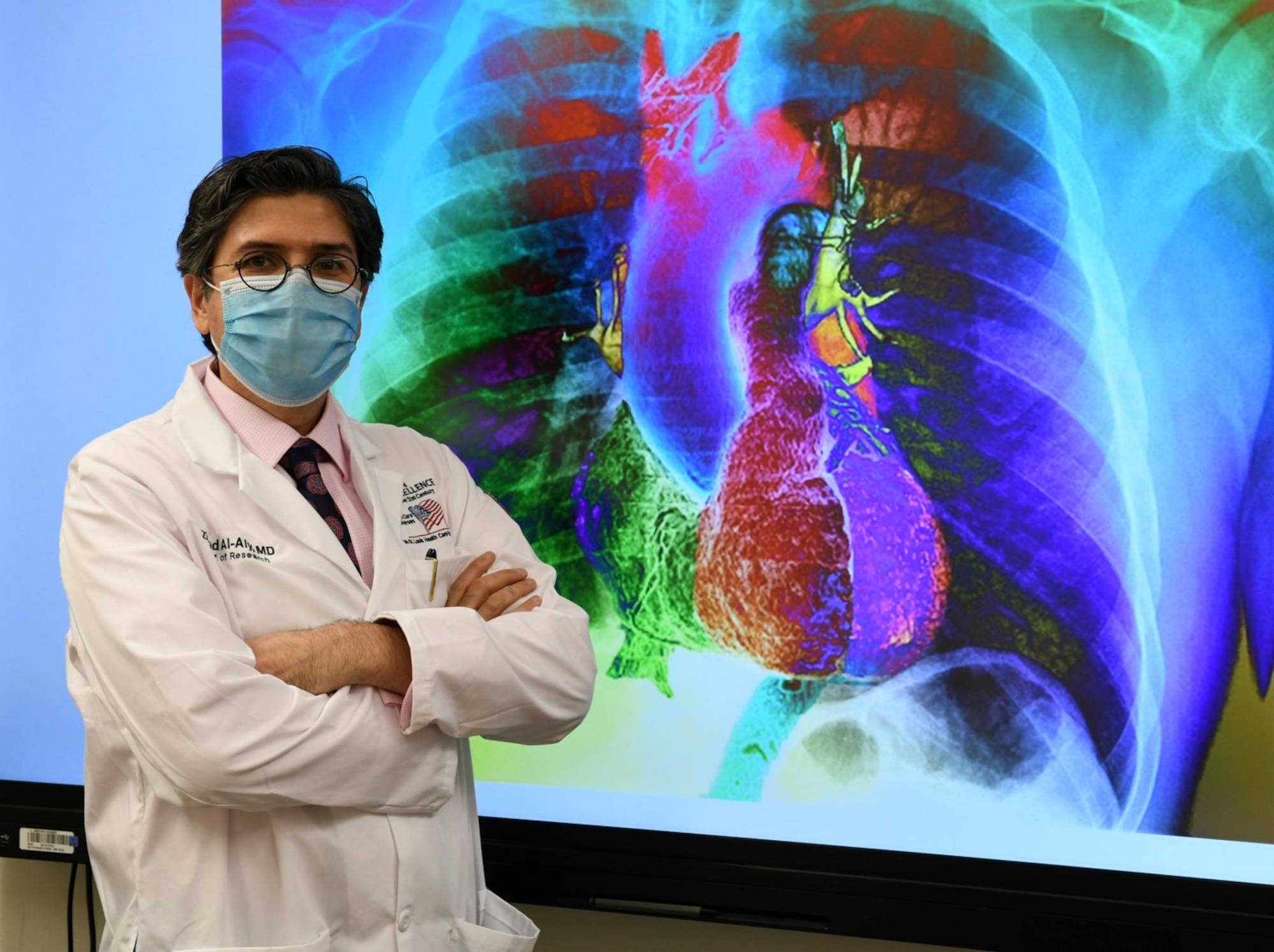
<small”>Ziyad Al-Aly, who holds positions at Washington University in St. Louis and at the Veterans Affairs St. Louis Health Care System, is not unaware of the criticism surrounding his research. He’s also willing to brawl, at times suggesting that many of his critics lack the expertise to evaluate his work or produce good research of their own. Visual: Mary-Dale Amison/VA
According to Al-Aly, VA samples can speak to the broader population. While it’s true that VA demographics don’t perfectly mirror the rest of the U.S., it’s reductionist to dismiss the findings on these grounds, he said. The average age of VA patients is about 60, but this figure represents a large distribution, said Al-Aly. And while women are about 10 percent of the VA’s population, this can translate to more than 600,000 people in a VA study. “We can fill 10 — 10! — Taylor Swift stadiums” with women, he said, which makes it possible to look for sex differences in their findings.
He also said they adjusted for differences in testing and access to testing over time. This would substantially reduce any bias if it existed, said Al-Aly. (The VA team adjusted for “a huge list of confounders,” said Morris, when commenting on the study of neurological and psychiatric outcomes.) “But having said that,” said Al-Aly, now speaking specifically about his group’s reinfection study, “it’s not unreasonable also to interpret the study, ‘these are the results, and the results really reflect the people who actually tested.’”
Nonetheless, Al-Aly said, knowledge from VA studies can be applied to the general population.
Speaking with Undark, Eric Topol pointed to a May Substack post that he co-authored with Al-Aly. It highlighted a number of studies that he described as aligning with the VA research. One was an EHR-based study from Italy, which found that people infected with Covid-19 had elevated rates of cardiovascular problems even three years after infection. (The study did not distinguish between Covid-19 patients who were hospitalized vs. not hospitalized.) The post also described a longitudinal study of patients who were hospitalized with Covid-19 in Wuhan, China. Three years after their initial infection, more than half reported at least one symptom, most of which were mild to moderate.
Long Covid, said Topol, is “prevalent. It doesn’t go away normally. There are some people that are lucky that they fully recover, but most kind of limp along.”
Like Topol, Al-Aly also said that long Covid recovery is rare, particularly among people who have significant post-exertional malaise or fatigue that lasts more than several months. Clinicians are not seeing recovery in these patients, he said.
Although Al-Aly was one of many co-authors on the Global Burden of Disease’s systematic review that found most people do recover, he said that the findings need to be interpreted with caution. The review’s primary goal was to track symptoms, not recovery; and even then, the study did not track all long Covid symptoms. Additionally, the review drew from a wide variety of studies — some based on surveys, others on clinical assessments, and yet others on information in databases. This is not the best way to assess recovery, he said, because long Covid symptoms sometimes come and go. A person may have brain fog that lets up for a while, only to return later. The best way to assess for recovery, said Al-Aly, is to follow people over time, checking in every three months or so.
(“That is an interesting point of view,” Vos wrote after Undark shared some of these concerns with him. “I think we had enough studies in our 2022 paper to reject the hypothesis of no recovery.” He added that his research team is currently working on an updated analysis: “It does look like there will be a small subset of people who remain symptomatic years after infection.”)
Later, when asked by email about specific critiques involving negative controls, Al-Aly described them as “grossly unfair.”
In response to a separate email asking about the different statistical approaches used to make his Covid and non-Covid groups comparable, Al-Aly pointed back to the Israeli study, the Danish study, and the Global Burden of Disease study: “We are criticized for using negative controls,” he wrote. These other studies “don’t use any means of quality control. Quite ridiculous that you criticize us for doing the right thing and elevating the rigor of the work.”
The scientific debate over long Covid has unfolded amid undeniable human suffering. Across the country, clinics have reported handling an influx of cases since 2020. Previously healthy individuals may suddenly find they need to sleep 18 hours a day. They may struggle with brain fog and breathlessness. Many people have had to scale back on work or quit their jobs entirely. Specialized care is often difficult to access, particularly for Black and Latino patients.
A post-viral condition can steal your whole life, a patient advocate told Undark. In severe, or even moderate cases, “you’re stuck in bed all day, you lose your friends, you lose a lot of your family, you lose your jobs, you lose your aspirations for life. If you wanted to have kids, if you wanted to get into a relationship, if you wanted to start a business, if you wanted to continue a hobby — all of that is gone.
“You’re just kind of suspended in life and dependent on the outside world to come to your rescue,” the patient advocate continued.
Those patients often find themselves facing skepticism from people who do not believe the condition is real — including, in some cases, their own doctors. And they are navigating symptoms at a time of intense political polarization over the implications of Covid-19.
The idea that long Covid is widespread, and that its numbers are growing, can be comforting for long Covid sufferers, said the patient advocate, who spoke on condition of anonymity in order to avoid blowback from within the patient community, which the advocate said, views Al-Aly as a god-like figure.
“He is beloved by patients. And I’ll tell you why I think he’s beloved by patients: because patients feel left to rot and die, and he has told them what I think some people interpret as a scary story, which is ‘long Covid is rampant. Everyone’s going to get long Covid. It’s going to disable the population,’” the advocate said. “To a patient, this is not a scary story. To a patient, this is actually a very hopeful story because everyone’s going to get sick; they’re going to have to help me.”
But the advocate expressed deep misgivings about promoting exaggerated views of the number of people at risk of developing long Covid. Such views won’t “help to have you taken seriously by skeptical people.”
For now, U.S. public health authorities — drawing on the research of Al-Aly and his colleagues — have continued to trend toward the broadest possible definition of long Covid.
The recent National Academies of Sciences, Engineering, and Medicine report recommended a new definition of long Covid for the U.S. government and health care system. The final result looks remarkably similar to Al-Aly’s description of the disease: Long Covid can be mild to severe, the report states, and it may include just one symptom or a single new diagnosis that develops after a SARS-CoV-2 infection and persists for at least three months.
In practice, this means that if a person has a mild case of Covid — say a cough and fatigue lasting one week — and then develops a chronic condition like lupus six weeks later, this new lupus patient could also be diagnosed with long Covid. “Clinicians must exercise their judgment and rely on evidence in reaching a diagnosis in any individual patient,” wrote Harvey Fineberg, a prominent public health expert and chair of the report, in an email to Undark.
Fineberg pointed to electronic health record data suggesting a large jump in rates of lupus onset after a Covid-19 case. Given that, he wrote, “a clinician would be wrong some of the time, but they would be more often wrong if [they] failed to ascribe the condition to long Covid.”
The long Covid diagnosis, Fineberg added, could help patients understand where the lupus came from, and perhaps in the future suggest treatments.
Public health expert Harvey Fineberg chaired a recent report which offered a new definition of long Covid. Fineberg stressed that “clinicians must exercise their judgment” in reaching a diagnosis.
But Putman, the Wisconsin rheumatologist, who treats lupus patients, noted that not all studies have found such a strong connection between an infection and lupus. He pointed to 2023 paper that actually found a protective effect of Covid-19 against lupus. “Do I believe that? No,” he wrote in an email. The real issue is “the data in this area are all very uncertain and often contradictory.” It’s implausible, he added, that the majority of new lupus diagnoses have been driven by Covid-19 infections. If this were the case, “we would expect a dramatic increase in the yearly rate of new lupus diagnoses. As far as I can tell, the incidence is more or less stable.”
Putman added that it would be difficult to run an effective clinical trial using a broad definition. The study participants would likely have multiple underlying pathologies, he said, that don’t all respond to the same treatment.
This new definition may also undermine the real and profound suffering experienced by some people with post-viral illness, said Leonard Jason, a psychology professor at DePaul University who has long studied ME/CFS, a severe condition marked by life-altering fatigue. “If a person has trivial pain in the toe for 3 months following Covid infection, with no negative consequences to the person’s functioning or quality of life, that person would still be eligible for a long Covid diagnosis,” he wrote in a recent opinion piece for Medpage Today. It’s a mistake to ignore symptom frequency and severity, he wrote.
The report recommended that the definition should be reviewed and possibly updated in no more than three years’ time, as the science continues to evolve.
“During the pandemic, the quality of research went down,” said Anders Hviid during a May Zoom call. “I think some scientists and probably also journal editors became a little one-sided or blind. Maybe it was because it became so polarized. So, people were either in one camp or the other.” There’s no question, he continued, that harmful symptoms can follow Covid-19 infections. But conversations about the frequency of those symptoms seemed out of touch, he suggested, particularly as time passed and the risk of developing long Covid declined as people acquired immunity.
Makam, in San Francisco, meanwhile, has spent years studying long-term health outcomes of people with prolonged serious illnesses. He worries about the consequences of having a poor case definition for long Covid. “How can you study a disease if you’re defining your illness very, very broadly, including a lot of different pathologies into this one disease syndrome?” He was blunt in his assessment of the work coming out of the VA St. Louis. “We’re going to look back and that entire line of work is going to be wrong. Like very wrong.”
Al-Aly’s third interview with Undark took place on May 30, the day Nature Medicine published his three-year follow-up study of patients with a documented Covid-19 infection in 2020. He had been up late the night before, putting together a thread on X, the platform formerly known as Twitter, with key points. It wasn’t all bad news, he wrote. Over time, people in the infected group became significantly less likely to die or develop new onset disease. Yet even three years out, those with mild infections remained at increased risk for some new onset symptoms.
He also expressed frustration with some of the criticism that has come his way, particularly on social media. “Good scientific criticism can sharpen the focus of the inquiry and make it better,” he said. But all too often, the critiques don’t serve any clear function and may even feed into denialism. “A lot of people feel sick and tired of this pandemic and want to move on, which is totally, totally understandable. Like, who doesn’t understand that? Who doesn’t sympathize with that?” Still, he said, the fact remains that many people need help, and he plans to help them — his detractors be damned.
“To the chagrin of the critics, we’re going to keep moving the ball forward,” Al-Aly said. If that irritates people, they’ll just have to get used to it, he added. “We’re working day and night to solve this problem.”


Though I haven’t read everything, IMO, one of the difficulties with long Covid is that there are, quite probably, many different long Covid diseases each one with different symptoms, disease markers etc. This might depend for instance on which parts of the body/brain the virus spread but compound that with different health backgrounds etc. This is not to say common or frequent markers cannot be found but it makes difficult even to define the group of diseases.
Yes, exactly.
I posed the same.
Lung fibrosis will not generate the same biomarkers as an autoimmune condition, and it may well be, in fact it does look like it, that even the autoimmune conditions triggered by COVID are not all the same.
Thanks, Yves, for posting this. And also for the shout out to ME/CFS, which I have had for decades now. Several thoughts in no particular order:
Sadly the belief that ME is psychological is far from dead. Just last week another young woman passed away after allegedly being treated in hospital as though her illness were her fault (as far as I can tell she fought for total parenteral nutrition but at some point gave up and opted to starve to death rather than continue to suffer–even when, at the 11th hour, TPN was authorized).
And then there was the NIH intramural study, which I gather is a bit of a Frankenstein’s Monster in that it has some useful data but also prominently features, for no reason patients can understand, “exercise preference” as a prominent concept. Patients have not been happy. There may be an inquest. If I were in the long covid community I would be very concerned that the same shitty researchers behind “exercise preference” and the PACE trial would bring their snake oil over to Long Covid Town.
Regarding Biomarkers: Apparently there are several promising ones for ME. None are widely used or accepted though. The one exception may be the two day CPET, where a patient intentionally makes themself worse, potentially permanently, in order to prove that their reactiin to exercise is different from someone who merely had not exercised much.
I am a particular fan of Ron Davis’ nano needle as a potential fiagnostic tool. Unfortunately, his application for funding was denied on some strange grounds like, iirc, that his son had ME so therefore he would be biased. As far as I have heard it remains a potentially promising biomarker, even if it might not rule out other some other causes of fatigue which would, I assume, need to be ruled out separately.
I mention all of this partly because these biomarkers might also help with long covid and I am not aware of anyone looking at that. And I can’t see why we shouldn’t.
On definitions: As the article said, the tug of war here is between patients and their advocates who feel that one disabling symptom should be enough to get approved for disability, and researchers who get frustrated by data made unreliable by the inclusion of a lot of people who technically fit the definition but whose illness might be entirely different (ie untreated b12 deficiency or iron deficiency). Both concerns are valid, and it makes me think that perhaps we should have a broader legal definition and a more narrow one sometimes used in research
One final thought or question: Of all the studies mentioned the Danish study did sound like it might potentially have the least bias in terms of counting covid infections, since they tested everyone who went out in public. Al-Aly dismissed it but didn’t provide any details. I wonder what his critique is?
Several things to note here:
1) Long COVID and SARS.
Once again one of the foundational sins of the pandemic is manifesting itself. Thousands of words and not a single mention of the original SARS outbreaks in 2003. It’s as if it never existed or it had nothing to do with COVID. When it is in fact a closely related virus, with largely the same properties. Just much more severe.
Had what happened in 2003 not been completely ignored, there would be very little controversy about LongCOVID. In fact everyone would have been quite certain LongCOVID would be a massive problem on January 1st 2020, i.e. the moment it was announced this was another SARS virus.
Because SARS patients back then developed something very similar to COVID, just at much higher rates and with on average greater severity. And they mostly never recovered.
2) This incredible howler:
Of course, the answer to this puzzle is that this isn’t a simple respiratory virus. It is a systemic infection.
And had that “expert” done his homework about SARS viruses, he would have known that. But he still hasn’t five years into this…
3) Biomarkers.
Because it is a systemic virus, the mechanisms behind LongCOVID are very diverse. So it is not unexpected that there aren’t consistent biomarkers. You have direct cytopathic damage to various organs — lungs, obviously, but also hearts, kidneys, etc. You also have more indirect damage through other mechanisms (looks like that is what happens to neurons in the brain). And you have general immune dysregulation. And most people only suffer some of these. Clear common biomarkers are most straightforwardly derived from the immune dysregulation. But again, far from everyone gets it the same.
4) Conflicts of interest.
Where do we start here…
Back in 2020 there were still some people in the public health/epidemiological/virological/medical communities that still had integrity and wanted to solve this problem. Five years later their number has dwindled greatly. The big names know what the political mandate is and what lines have to be followed, if the inflow of grants and awards is to continue. So they are not going to go out publicly telling everyone how we just infected everyone several times and are strongly committed to infecting everyone endlessly with a virus that causes permanent damage to a substantial proportion of people on each round. That would be as clear example of a monstrous crime against humanity as there has ever been, right? But out political elite consists of pure and innocent people who would never do such a thing, right…
All of this is well stated as usual, but point 2) really gives the game away here. Calling SARS/Covid a “simple respiratory virus” immediately discredits the “expert” in question and shows that said expert is as susceptible to the politicisation of the problem as the vast sea of normies. It is no more a “simple respiratory virus” than measles.
Put another way, if you had asked a specialist in a relevant field in, say, the first half of 2019: “Was SARS/is MERS a ‘simple respiratory virus’ there were only two possible answers to that question: “no, obviously not” or “I don’t know”. If one answered the latter, they could acquaint themselves with some of the literature in about a day and come back answering the former.
(Some hypothesised early on that after ~immunity~ that SARS2 would become a mere simple respiratory infection, sometimes with reference to OC43, hypothesised to have become a common cold virus after causing a pandemic in the late 19th century. Evidence for this historically and contemporarily remains thin-to-non-existent.)
this speaks to GM’s point 1), the total ignoring of the SARS1 literature in this and almost all similar articles, which, crucially, was not a politicised disease. SARS2 is closely related to SARS1.
The other point is how this article totally ignores the many studies demonstrating observed pathological damage in SARS2 survivors – not all, but enough to be a serious problem. These have been shared repeatedly here. The most striking is brain injury. There’s also the lung damage question – ie recall the case of the 50-something tech billionaire who injects himself with unicorn piss or whatever because he’s afraid of aging having his lungs shredded after a “mild” omicron infection. He only knew this, of course, because he’s rich enough to have advanced medical imaging on tap. That the article focuses on Al-Ahly’s more epidemiologically-oriented studies while ignoring the immense body of complementary literature on the specific mechanisms of potential harm of this disease is clearly a deliberate tactic.
Finally, briefly, the article leans on “muh immunity” gospel. a couple of anointed experts toss out the “this will become less of problem going forward because immunity” which is obviously just made up, and in fact ignores a specific Al-Ahly study showing increased risk of LC with subsequent infections using real world data.
The purpose of the article is to prime Undark readers, using a fairly thin veneer of journalistic impartiality, to react with either “aha! bullshit!” or, “probably nothing to worry about” the next time new Al-Ahly research is publicised. This isn’t to say he’s infallible (and by the way, quoting an anonymous long covid patient to try and stitch Al-Ahly up with “the community treats this guy like some kind of god figure!” is so pathetically transparent), but nor is he the first and last word on the scale, scope and specifics of this problem which is very obviously a very big one.
How can an article this exhaustive about long covid never mention the possibility that the Covid vaccines may play a role in it as the vaccine makes the body produce a longer lasting synthetic spike protein? The spike protein being recognized as the main pathogenic feature of the covid infection. Also there is the fact that the nanoparticle coatings of the synthetic mRNA delivered by the vaccine can also cause distress in the body.
Because large-scale studies consistently shows that getting vaccinated reduces the incidence of Long Covid.
Moreover, vaccine uptake has fallen off a cliff while Long Covid prevalence continues to rise.
Moreover, data from countries that had formerly contained and eliminated the virus and therefore had relatively distinct periods of mass vaccination followed by mass infection, show increased prevalence of long covid and other noticeable population-wide indicators of adverse health correlating strongly with the period of mass infection, and not with mass vaccination. Like, at all. NZ shows this most clearly. Australia too to a lesser extent (greater overlap here between mass vaccination and mass infection in the 2nd half of 2021 in some states.
Moreover, there were trials of the vaccines before they were deployed. These were relatively rapid, due to the acute nature of the crisis, but the fact remains that there was no report of anything like a statistically significant emergence of a long covid-like syndrome in the trial data. There were reports of vaccine harm in VAERS once the vaccine was deployed, but on top of all VAERS’ usual limitations, the data is fairy useless as it is confounded with basically unrestrained mass infection in a country where the disease and vaccine were both hopelessly politicised, including among MDs. On the other hand, in Australia, as soon as AstraZeneca was showing a slightly discernible increased risk of clotting (which is one manifestation of LC) in certain age groups after it was deployed, its access was greatly throttled (and it is of course no longer available).
Vaccines are not causing this problem, and “but teh spike protein!!”, while it is certainly, shall we say, a talking point is a meagre and unpersuasive argument to the contrary. This blog primed me in 2020 to entertain the possibility that the vaccine would be Literal Poison as a consequence of a rush job from some of the most untrustworthy companies on the planet. It’s not. That’s unambiguously clear.
The doomed-to-failure vaccine strategy, however, was the wrong one, and has had disastrous consequences since early 2020, vaccines being both unnecessary and insufficient to solve the problem of SARS-CoV-2. Selling the covid vaccines as on a par with the vaccines that changed the course of human history, in spite of the decades of literature showing poor performance of vaccines against coronaviruses, was, besides itself being a de facto anti-vax policy (although the out-and-proud covid anti-vaxxers, themselves being every bit the abject and inane conformists as the vax-and-done crowd, are too stupid to even begin to grasp this), an outrage that has been used to rationalise mass death and illness at an unconscionable scale, and redirect the electorate’s anger to the paltry and inept attempts of most states to reduce this burden of human suffering during the acute stage of the crisis. That all said, I have no regrets about being vaccinated and will readily get vaccinated again should the circumstances call for it (not bothering atm because NPIs have been extremely effective for me and there are no meaningfully up-to-date vaccines available so it’s not a particular priority for me at the moment).
Thanks for a very clear exposition of the issues.
It is of course possible that individuals can suffer from vaccine damage while the population as a whole benefits. I know at least one person who likely suffered vaccine damage. I was very sceptical at the time (I assumed that she had just got covid coincidentally with the vaccine and was suffering long covid), but the more I find out about her case the more likely it is to me that she is one example of vaccine damage. But as you and Yves have pointed out, study after study indicates that at a population level, vaccines do provide significant protection/mitigation of long Covid.
What is infuriating of course is that it seems that all public health authorities are just focusing on giving vaccines seasonally to the vulnerable, instead of systematically investigating how they can be used (along with all the other mitigations we know about), to minimise the damage covid is doing to us all.
Just to add one point on SARS1. Its not just the long covid potential of the virus that was memory holed. There were also plenty of studies at the time of SARS1 that strongly pointed to it being an airborne virus. From memory, there was a very good study from Hong Kong that proved that it had moved through an apartment building via the ventilation/sewerage system. This was, of course, completely forgotten about by 2020.
GM,
Thanks for that very clear summary of quite probable and justifiable reality.
“It’s just difficult to imagine that a simple respiratory virus could be so detrimental to all organ systems at a population-level scale,” said Hviid.
In my view, this is the problem – SARS-COV-2 is not a respiratory virus. It is a virus that attacks the vasculature and can damage blood vessels throughout the body and so affect every organ system. This will account for the myriad symptoms of long covid. Furthermore, the damage might be progressive and symptoms might not occur rapidly, but only emerge as *new* symptoms some period of time after an apparent recovery from the infection.There are now very many reports on the endothelial dysfunction and thrombotic effects of Covid-19. (For example: Xu et al., 2022 “Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies”) The most frequent route of ingress is via the respiratory system causing damage to the hyperfine vascularization of the lungs. Thus, respiratory symptoms are common and this has lead, in part, to the notion of it being a respiratory virus. The other reason is likely it being a coronavirus – the same virus family that common cold viruses belong to. But, barking up the respiratory virus tree is not helpful because it drags along with it strong biases about what respiratory viruses can and cannot do as exemplified by Hviid.
I had an asymptomatic wild type infection somewhere in January 2020(!). At the time I was healthy, ran 25 km a week and lifted weights regularly. By the end of 2020 I could no longer run or lift weights without getting post exertional malaise (no shortness of breath, no sore muscles, but 6 to 48 hours after exertion appear chest pains, fatigue, impaired balance, brain fog and this can take more than 3 weeks of rest to abate). I had also experienced many different symptoms that fluctuated in severity and onset. These included a (permanent?) loss of sensation on the soles of my feet (small fiber neuropathy), tinnitus that might last for several weeks and then disappear only to reappear a month or two later, impaired olfaction, chest pains (the cardiologist could not see any problem), brain fog (memory problems, cognitive problems), impaired balance, excessively prominent veins, “covid toes” due to pooling of the blood in the feet, hair loss, sleep difficulties, dyslipidemia (all other blood tests normal), microclots confirmed with fluorescence spectroscopy, joint pains, and there are more. New symptoms emerge out of nowhere. Others seem to disappear. Fortunately I am not bedridden as some others are and I can still manage to look after myself. But I have noticed a steady decline in overall health over the past 4 years of long covid. I have also never tested positive for SARS-COV-2 (PCR for nucleocapsid, nasal swab for spike protein by pharmacist, numerous rapid antibody tests for spike protein) yet there is no other reasonable way to account for the symptom onset and range other than ascribing it to Covid-19.
If, as I understand current thought, Covid is a vascular disease that can cause damage throughout the body, alters the immune system, has been demonstrated to invade the brain, and can lay dormant for years before rampaging a la HIV, then the manifested harms will be legion and many may already be baked in. At least medical professionals are masking and building ventilation has been improved (sarcasm alert). I hope research leads to better treatment for those suffering today from Covid damage and others that will be joining their ranks. While we still have enough people with most of their cognitive functions intact.
I think Yves is too kind. I don’t see mere arrogance, I see obfuscation.
We’re drowning in strikingly various evidence for persistent organic disease(s) post-covid, and have been since early in the pandemic. In this context one should anticipate that sorting out correlations and causes will be difficult, even bewildering. Epidemiologists using this as an excuse to ask “Is it real though?” are beneath contempt.
this is an exceptionally well written article. Nuanced and insightful. It speaks to the enormous challenges of even good people doing quality research on a nebulous illness.
Just the matter of disease definition: it isn’t so much who is right or wrong, but what gets missed depending on how wide or narrow you define the illness.
Re: it seems to be unduly inclined to take the point of view that there must be biomarkers, a well-understood pathological process, and/or a tidier set of symptoms
You have hit the nail on the head Yves. Conventional MDs simply can not seem to grasp gray areas- if there is not a well known clear cut test with a binary positive/negative, or high/low, pointing clearly to a straightforward diagnosis, they refuse to acknowledge it. CFS/ME is correlated with high IgG antibodies to EBV, CMV, HHV-6. But because almost everyone carries a viral load, and not everyone ends up with chronic fatigue, most doctors refuse to think those results are significant when a patient is symptomatic. Despite the fact that when these patients are treated for these viruses, it does indeed improve their symptoms. And yes there are pubmed studies out there pointing out that even without IgM antibodies to these herpes family viruses, IgG load can causes symptoms and should be addressed (but for whatever reason these types of studies get ignored).
And we know now of course, that Covid can also reactivate viruses such as EBV and cause chronic fatigue and/or fibromyalgia symptoms even in people who never had these issues before.
As Ignacio mentioned, Covid will manifest in different ways in different people. But this doesn’t fit into the cookie cutter paradigm of the allopathic world where x disease means you get x drug and this works for all patients with x disease.
A patient told me she waited for months to get into the long covid clinic and has seen specialists there for about a year but feels they don’t communicate well and she is getting confused between all the medications and supplements she is now taking. Her latest inquiry was about how her long covid doc feels she could try an SSRI since that seems to help some of the other long covid patients. Her psychiatrist said well you are already on another anti-depressant, starting an SSRI can cause more side effects, why don’t you take St John’s Wort instead. She asked me what I thought: 1. Your long covid doc seems like they are shooting in the dark but sure we can try some serotonin support 2. I’m very surprised your psychiatrist recommended St John’s Wort. Many herb-drug interactoins are overblown but this is a very well known and legitimate one and considering how many pharmaceuticals you are on, this is not the best idea. 3. We can add in cofactors and precursors to serotonin to your treatment plan that will not interfere with your medications instead if you prefer.
She also got the recommendation from either her PCP or long covid doctor to get a Covid booster. She had a severe reaction to the mRNA vaccine in the past- I’m sure you can guess which one they had her get, not even bothering to mention any alternatives like Novavax. And all of her symptoms flared badly for weeks. It is frustrating to see “experts” in “expertise” clinics bumble around and I feel for these patients. They are not getting the guidance and treatment they deserve.
Looks to me like “don’t catch Covid” remains priority #1 for those looking to avoid disability or worse.
Thanks much for this piece Yves. The gaslighting from the medical community is infuriating.
“It’s just difficult to imagine that a simple respiratory virus could be so detrimental to all organ systems at a population-level scale,” said Hviid.
According to some it was designed to do just that, ie “gain of function”.
My neighbor’s son-in-law and I both have long COVID. As he put it, “there’s your life before LC and your life after LC”. Others, like the guy who delivers our propane, says that he now becomes exhausted after half a days work. The Facebook LC support group is full of very sad stories – many people much younger than myself are completely debilitated, at least I can still get out of the house and do things. Many of these people still have to work.
My local MD has referred me to a physician in Seattle at the University of WA hospital who is treating LC patients and running a study. I’m wondering if it will be worth the trouble of driving down there (60 miles of heavy traffic) to see him but I may give it a try at least once and see what he has to say.
For remedies, I am trying all kinds of things – Chinese herbs, acupuncture, supplements etc. Currently I am trying nicotine patches as there is a very small study that indicates that nicotine may bind to the same cell receptors as coronvirus spike proteins.
https://europepmc.org/article/PPR/PPR552490?javascript_support=no
I’ve only been on them for 4 days but it seems to help.
Even before my husband and I got Covid together in February 2021 — we were sick at the same time for six whole weeks — and subsequently Long Covid up until now, I got solid information and analysis from Dr. Roger Seheult on MedCram. He is a pulmonologist and medical researcher that has been treating Covid patients since the beginning of the pandemic, and very soon he made it clear this is a systemic illness that causes significant and lasting vascular and immunological damage on the body.
While some individuals in the scientific community keep debating the merits and nuances of a Long Covid diagnosis, etc., as they fight for grants and notoriety amongst themselves, patients like my husband and myself deal with the day to day realities of this condition. We are lucky to have access to an excellent Long Covid program in NY (at Mt. Sinai) where we see doctors that treat us in validating ways, working with us as a team. We are also lucky to be able to compare our experiences with one another and observe our progression, and help each other manage our symptoms with love and compassion. The human aspect of Long Covid is extremely important to deal with it.